Introduction
Renal elimination is a normal physiological phenomenon that provides information on the functioning of the body. The absence, reduction or exaggeration of elimination indicates an abnormal or pathological state of functioning of the body. However, several factors can cause a disruption in this function. This is the case with age. It is indeed estimated that the evolution of age can Articlecause disruptions in renal function, thus leading to urination disorders, including incontinence [1]. Thus, many elderly people feel the need to empty their bladder at very regular intervals. This time interval is singular and depends on several factors that can be of physiological or psychological origin [2]. Indeed, while some people urinate abundantly, others urinate in small quantities, in jerks or residually [3]. In addition, the urgent or pressing nature of the need to urinate depends on several variables. It depends on the location, circumstances, proximity to the places of urination, the presence of a third person, etc. It is common to hear people complain of loss of urine when near a toilet. Others experience an irresistible and very pressing need to urinate as soon as they are near their home. This phenomenon causes subjective suffering and sometimes shame for the person. The variabilities observed in the manifestations of this problem indicate that these determinants are not only physiological [3]. This raises the problem of the determinants and repercussions of urination disorders, including urinary incontinence in the elderly. From the worrying nature of this problem, its psychological determinants and its implications on the lives of the elderly, it should be noted that among the usual pathologies in senescent people in internal medicine, urinary incontinence figures prominently. Monod reports that in the United States of America, urinary incontinence is associated with functional decline and the risk of institutionalization [4]. Monod estimated that it presents more than 70% risk of being institutionalized during a two-year follow-up [4]. Also, Monod reports that urinary incontinence is associated with the risks of decline in mental health with the occurrence of anxiety or depressive disorders [4]. It also causes a decrease in quality of life, self-esteem and a limitation of the participation of elderly people in social activities. Monod recommends that efforts be made for early detection of this disorder in order to reduce the psychological suffering of these people [4]. In terms of the prevalence of urinary incontinence, this pathology evolves in the growth with age, especially in women over 75 years old. Deffieux, it is illusory to consider urinary incontinence as a disease of senescence [5]. Deffieux reported at the end of his study that approximately 10% of women under 25 years old suffer from urinary incontinence. For this author, urinary incontinence increases with age, it is more frequent in senescent people than in other social categories. Cahill showed that urinary incontinence affects the quality of life of those affected more harmfully than any other chronic pathology [6]. Thus, under a dread of prejudices, the elderly is fearful and constantly stressed. Women living with incontinence are likely to suffer from reactive depression. In addition, incontinence impacts every aspect of a person’s life. It disrupts social relationships, sex life, ability to work, travel or play sports and participation in community life.
In Benin, addressing the issue of urinary incontinence is not an easy thing for the subject or for his family circle. This difficulty seems to have a lead effect on the country’s health system. Indeed, the synthesis of documentary data on urinary incontinence shows that this disease is very less investigated in the Beninese context. The most investigated health problems among the elderly are related to prostate cancer and obstetric fistulas. Incontinence is not yet a major source of concern for health policy stakeholders in Benin.
In addition, the elderly, due to limitations (mobility, language, resources, etc.) are forgotten by the actors of the health system policies. In hospitals, their support is experienced as a chore by health workers and auxiliaries. For others, it is a waste of time. In addition, families, due to sociocultural reasons, mostly resign. This exclusion linked to the weight of dependency and culture is also aggravated by other sources of discrimination and marginalization, such as labeling.
The fight against this serious discrimination is urgent in several respects. First, because the denial of the right to psychological support deprives the elderly of the opportunities for an active retirement and the benefits of perfect health. Too often, the trivialization of the needs of the elderly in primary health care strategies and psychological support marks the beginning of mental disorders leading to severe forms of psychopathology. It therefore appears that urinary incontinence is a serious health problem that particularly affects the elderly. Support and care strategies are less highly rated in care strategies in Benin. Faced with this problem and in this context of precarious living conditions, it is important to ask how psychological factors affect the quality of life of the elderly facing urinary incontinence.
Old age is an issue that concerns everyone because everyone will grow old or has an elderly parent. With the advent of the phenomenon of birth control or regulation, the population of elderly people is constantly increasing. It would be the social class that is experiencing a dizzying increase. In 2015, the size of the population of elderly people was estimated at 382,587 in 2011 while it was 374,549 in 2002 [7]. Globally, the population of over 60s was 694 million in 1970. It is estimated that this population would be 1.2 billion elderly people in the world in 2025. World Health Organization (WHO) forecasts indicate that in 2050, the number of elderly people would be around 2 billion [8]. About 50% of these people would live in developed countries. Thus, the level of development of the country improves the life expectancy of the populations. However, in developing countries, life experience has started to increase considerably. The aging of the population constitutes a development problem, because people are physically diminished and produce less or on the contrary become like children, passive consumers. On the physiological level, it is estimated that aging leads to a decrease in physiological mechanisms with a dampening of the various functions. In terms of bladder function and the entire urinary system, with aging, there is bladder compliance, a decrease in the contractility capacities of the detrusor with sometimes involuntary contractions, urethral pressure, prostatic hypertrophy, vaginal and urethral atrophy and predominantly nocturnal urination (nocturia).
Also known as functional urinary disorder, voiding disorders, lower urinary tract symptoms are numerous. They include all the warning signs of a lower urinary tract dysfunction. Knowledge of these symptoms by the practitioner makes it easier for the latter to describe the patient’s voiding pattern based on their complaints. To do this, Lower Urinary Tract Symptoms (LUTS) are classified into three groups, namely: Storage phase symptoms, voiding phase symptoms and post-void phase symptoms. There are nine types of urinary incontinence defined by the Industrial Control System (ICS) in 2017. These are Stress Urinary Incontinence (SUI); urge incontinence (a sudden, compelling and irrepressible desire to urinate. This is a pathological need that is different from a strong urge to urinate, especially because it does not warn); mixed incontinence (it represents both stress urinary incontinence added to urgency); dysuria or dysuric syndrome (delay in starting urination, need to push to initiate urination, weak and/or watering can stream, interrupted stream and urination in several stages); enuresis (involuntary complete urination); daytime pollakiuria (increase in the number of urinations per 24 hours; nocturia awakening induced by the need to urinate); clinical syndrome of overactive bladder; bladder sensitivity (reflects a need to urinate progressively increasing until a pressing need is obtained).
These disorders come from the damping of cells and urinary functions. The damping of this set causes urination disorders in the elderly. These disorders are generally not understood by young people who wrongly consider these difficulties of the elderly as a consequence of their wickedness. This misunderstanding constitutes a source of suffering for the elderly, because they are not adequately supported. This sometimes leads to isolation of the person, because their environment is not understanding. In some environments, those around them develop an extraordinary blindness to the suffering of the elderly and do not encourage either the call for help or the verbalization of the suffering felt and experienced painfully. In addition, these people generally do not have access to health care. They are generally unable to express their suffering. However, without the expression of the problem by the patient, the care poses an enormous difficulty. It is in view of this that Boddaert et al., considered that elderly people who do not communicate about their difficulties are vulnerable people [9]. Apart from this request for care or the late request for care, urinary disorders are delicate pathologies that impact the social functioning of the person. The management of urinary disorders including urinary incontinence requires special attention. If nothing is done, the patient may develop psychological difficulties that complicate their suffering in the face of the disease. It is common to observe comorbidity in elderly people, that is to say the simultaneous presence of urinary disorders and mental disorders, especially depression. It is in view of this that El Khoudri et al., considered that urinary incontinence significantly affects the physical, psychological, social well-being and quality of life of women [10].
Comorbidity situations are common among elderly people facing urinary incontinence. Given the difficulties experienced by elderly people facing urinary incontinence, they may suffer secondarily from psychological disorders such as anxiety, depression or even serious and disabling psychoses. Bruno et al., report that the prevalence of mental disorders among elderly subjects with urinary incontinence is between 3.2% and 14.2% [11]. They mention that in the manifestation of these pathologies there are singularities that must be taken into account in the treatment. According to Mareau et al., the behavior of some elderly people reflects an inexorable emotional greed and an eternally unsatisfied need for attention, often causing reactions of weariness in families and caregivers [12]. Faced with this observation, they concluded that the entourage of the elderly or the professionals who provide care to this category of person must understand this mental functioning in order to respond favorably so as not to push them away. The vulnerability of the elderly promotes the development of serious psychotic disorders. According to Le Rouzo physical and cognitive fragility, multiple sensory losses, isolation, emotional loneliness, hospitalization, are all factors likely to promote the appearance of psychotic disorders in the elderly [13].
Materials and Methods
This study is part of a mixed approach, combining qualitative and quantitative approaches for a better understanding of the phenomena studied. Although the research adopts a mixed perspective, the qualitative dimension predominates, with particular emphasis on the descriptive and explanatory analysis of micturition disorders and the psychological disorders they cause. The descriptive character aims to expose the different variables involved, while the explanatory character seeks to establish causal links between micturition disorders and psychological consequences in the elderly. Participants are chosen because of their direct or indirect involvement in the management of micturition disorders in the elderly. The choice of the study population was made in a reasoned manner, taking into account the patients registered in the urology and psychiatry departments of the academic year 2022 and 2023. The sampling was carried out according to the Cahill approach, which recommends that the sample represent 20% or more of the parent population [6]. Thus, a total of 92 participants were selected, including 40 patients, 40 family members, 2 doctors, 2 supervisors, 2 administrators, 2 social workers, 1 member of the control body and 2 clinical psychologists. The choice of interviewees was made according to their relevance to the research theme and their involvement in the process of healing or managing urinary incontinence. The study mainly targets two groups of patients: Those suffering from urinary incontinence and those who have developed mental disorders related to urinary incontinence. These patients are studied in order to evaluate the psychological consequences of their condition, with the aim of improving care and psychological support.
The main collection tool is the survey questionnaire and three types of questionnaires were developed for this study, each adapted to a specific group of respondents: Health workers, patients with urinary incontinence and their families. Each questionnaire includes three main sections: One on the activities of health services, one on the impact of these activities on the mental health of patients and one on the qualification of the staff in charge of patient care. It should also be noted that two scales were used. These are the Hospital Anxiety and Depression Scale (HAD) and scale Nurse’s Observation Scale for Geriatric patients (NOSGER).
The interview guide was designed to collect information from health workers and managers of urology and psychiatry services. This guide is structured in two main parts: A series of 13 questions on the impact of health services on patients with urinary incontinence and a section devoted to the socio-demographic characteristics of the respondents (gender, profession and function). In addition, the recording of interviews was used as a method of collecting empirical data to ensure the fidelity of the information collected. The recording sessions took place during interviews with patients, their families and health professionals, thus allowing a more precise analysis of the data collected.
A pre-test was used to assess the relevance of the questionnaires and interview guides before their use in the field. Once the tools were adjusted, the survey was conducted among the selected participants over a period of one month from July, 2023 to August, 2023. This phase consisted of administering the questionnaires, conducting the interviews and collecting data via the rating scales and recordings. The quantitative data, from the questionnaires, were coded and analyzed using statistical software such as Statistical Package for the Social Sciences (SPSS) (version 27). The qualitative data, collected via the interviews and recordings, were analyzed using thematic content analysis methods. This combination of methods allows for triangulation of the data, thus ensuring better validity of the results.
Results
Sample specification
This is the point of the different components of the sample using tables.
Sociodemographic data: The majority of survey participants are elderly people and their parents or relatives, each representing 43.48% of the total number of participants, indicating a high level of involvement of these groups in the phenomenon studied. Health professionals, including doctors, clinical psychologists and social workers, represent a smaller group, totaling approximately 7.60% of participants, suggesting a lower presence of these actors in the sample (Table 1).
Table 1. Summary of the sample according to social categories.
| Categories |
Staff |
Percentage (%) |
| Elderly people (active and retired) |
40 |
43.48 |
| Parents (descendants and relatives) |
40 |
43.48 |
| Supervisors |
2 |
2.17 |
| Doctors |
2 |
2.17 |
| On-call administrators |
2 |
2.17 |
| Clinical psychologists |
3 |
3.26 |
| Social workers |
2 |
2.17 |
| Control body |
1 |
1.09 |
| Total |
92 |
100 |
Supervisors, guard administrators and control corps form even more restricted categories, with numbers varying between 1.09% and 2.17%. We now turn to the distribution according to gender.
Distribution of elderly people encountered according to their gender: It appears that 23 or 57.5% of the elderly people surveyed with urination disorders are male, compared to 17 individuals or 42.5% who are female (Table 2).
Table 2. Distribution of elderly people encountered according to gender.
| Gender |
Staff |
Percentages (%) |
| Male |
23 |
57.5 |
| Female |
17 |
42.5 |
| Total |
40 |
100 |
Still within the framework of this work, our investigations allowed us to list the patients according to the age groups that we discover (Table 3).
Table 3. Distribution of patients surveyed by age.
| Age difference |
Staff |
Percentages (%) |
| Between 50 and 60 years old |
6 |
15 |
| Between 61 and 70 years old |
24 |
60 |
| Between 71 and 80 years old |
6 |
15 |
| Between 81 years and over |
4 |
10 |
| Total |
40 |
100.00% |
Distribution of patients according to age group: According to the archives of the various targeted services and the ancestors or relatives of the patients interviewed, we note that, 06 or 15% are in the age group of 50 to 60 years also 15% for the age group of 71 years to 80 years, while the age group of 61 years to 70 years includes 60% of the sample. The rest, 10% are between 81 years and over as shown in Table 3. This means that the population of patients received in these services is mainly of the 3rd age. These socio-demographic data allow us to have a general opinion on the study sample. In the rest of the research, the different types of urinary incontinence noted in patients were categorized.
Type of urinary incontinence observed in the subjects surveyed
The aim here is to identify the number of patients who are subjected to daytime or nocturnal urinary incontinence, whether permanent or otherwise due to trauma. The responses obtained to this concern are recorded in the following table.
Distribution of patients according to their type of disorder: Data analysis shows that urinary incontinence due to specific causes is much more common than ordinary urinary incontinence. Indeed, only 15% of patients suffer from ordinary incontinence, while the majority (85%) of cases are distributed between different types of more complex incontinence as presented below in Table 4.
Table 4. Distribution of patients according to the type of urinary incontinence expressed.
| Types of urinary incontinence |
Staff |
Frequencies (%) |
| Ordinary urinary incontinence |
6 |
15 |
| Nocturnal urinary incontinence |
4 |
10 |
| Daytime urinary incontinence |
2 |
5 |
| Permanent urinary incontinence |
2 |
5 |
| Urinary incontinence due to bladder sphincter deficiency caused by neurological disease |
12 |
30 |
| Urinary incontinence due to bladder sphincter deficiency caused by trauma |
7 |
17.5 |
| Urinary incontinence due to urethral sphincter deficiency caused by neurological disease |
8 |
20 |
| Urinary incontinence due to urethral sphincter deficiency caused by trauma |
5 |
12.5 |
| Total |
40 |
100 |
Incontinence due to bladder sphincter deficiency caused by neurological disease is the most common (30%), followed by incontinence due to urethral sphincter deficiencies caused by neurological disease (20%) and trauma (12.5%). Permanent and diurnal forms of incontinence each account for 5% of cases, making them less common forms. This distribution shows the importance of neurological and traumatic factors in the development of incontinence in patients, highlighting the need to identify the underlying psychological repercussions more closely.
Psychological impact
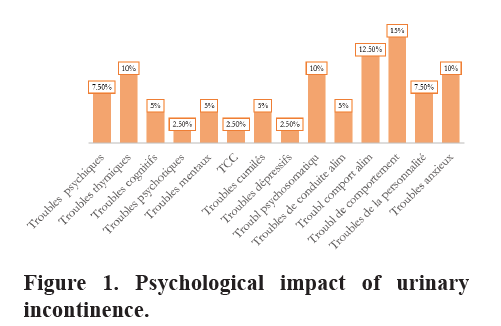
This is the stage of psychopathological aspects observed in subjects with urinary incontinence and/or micturition disorders. At this stage, the work consisted of examining the elements of psychopathologies underlying urinary incontinence and those caused by micturition disorders. To this end, the data collected from elderly subjects surveyed using the Hospital Anxiety and Depression Scale (HAD) and Nurse’s Observation Scale for Geriatric patients (NOSGER) scales, as well as the diagnoses obtained after consulting the archives of the urology department and the mental health department, made it possible to identify the psychological repercussions of urinary incontinence in elderly people of the 3rd age. These repercussions are represented by graph 1.
The careful analysis of this graph 1 of psychological impact of urination disorders shows that senior citizens in Cotonou, subject to urination disorders, have developed various kinds of psychological suffering. Indeed, according to this graph, 6 individuals or 15% of them are harboring personality disorders against 5 individuals or 12.5% presenting behavioral disorders. 4 subjects or 10% are prone to anxiety disorders against 3 others or 7.5% who suffer from psychological disorders. 12.5% have eating disorders 5% have eating disorders 10% of subjects sink into mood disorders while 10% of respondents suffering with psychosomatic disorders against 2.5 who are depressive. We also note 5% of cumulative disorders against 2.5% of obsessive compulsive disorders. 2.5% have psychotic disorders. While we recorded 5% for cognitive disorders as well as 5% of mental disorders.
Perception of urologists and mental health specialists in the management of urinary incontinence
The various professionals surveyed report various opinions regarding the care of the subjects. These opinions converge towards the same gap: The absence of complete care of patients.
Comments by specialist in urology, urologist: “For those of us who work here every day with patients who have urinary incontinence problems, we do our best with the means, tools and technology that we have at our level to try to help these people who suffer from these problems to get better on a daily basis. But it should be noted that our hands are also sometimes tied because the services offered are generally limited to the medical aspect. Which, for the well-being of these patients, is really very limiting”.
These statements show that the healthcare staff strives to provide adequate care to patients with urinary incontinence using the available resources. However, the limitations of the services offered focus mainly on the medical aspect, leaving aside aspects essential for the overall well-being of patients. The lack of consideration of psychological and social dimensions hinders the effectiveness of support. These statements are consistent with the opinions of Medical Technician (MT) for whom the technical platform present in the urology department is insufficient for the complete care of the subjects.
Comments by Medical Technician (MT), nurse: “The technical platform offered to patients suffering from urinary incontinence is considered insufficient, not fully meeting their needs. The speaker highlights the shortcomings in the current approach which is mainly limited to the medical aspect, neglecting other important dimensions for overall care. These patients often present symptoms that go beyond physical disorders alone, including psychosocial repercussions that are not sufficiently addressed. The social and environmental aspects of patients must be integrated into the care process. Better consideration of these factors could improve the general well-being of patients”.
The technical platform offered to patients suffering from urinary incontinence is considered insufficient, not fully meeting their needs. The speaker highlights the shortcomings in the current approach which is mainly limited to the medical aspect, neglecting other important dimensions for overall care. These patients often present symptoms that go beyond physical disorders alone, including psychosocial repercussions that are not sufficiently addressed. The social and environmental aspects of patients must be integrated into the care process. Better consideration of these factors could improve the general well-being of patients. Finally, a psychologist reports that it is rare that patients are sent home.
Comments by Mental Health service (MH), psychologist: “You know, complete care for patients with urinary incontinence-related disorders is normally multidimensional care, multidisciplinary care, not to say complete care, because this pathology, this urinary incontinence, has a lot, or generally has a lot to do with the well-being, not only physiological, but also the overall well-being of the person suffering from it and when we talk about overall well-being, we include physical health, psychological health, social well-being, social integration, engagement in social life, many elements and it would be really important, really necessary for these people to be followed up. However, even if we do receive cases in the psychology department, it must be said that it is really very rare. It is really very rare to be able to receive cases of this kind, people who complain of these pathologies and especially at the level of which we notice a lot of repercussions that can range from sleep disorders to depression and others. So it would be really important for complete care to be put in place to improve the condition of these patients”.
Urinary incontinence affects multiple dimensions of patients’ well-being, requiring complete management to address their overall needs. Treatment of this condition should include not only medical interventions, but also psychological and social care to improve quality of life. However, it is rare for these patients to be referred to psychological services, despite the emotional repercussions they experience, such as sleep disturbances or depression. This situation highlights the importance of multidisciplinary management for better management of incontinence-related disorders. Such an approach could significantly improve their overall well-being.
Discussion
Urinary incontinence in the elderly is a complex problem with multiple physiological, psychological and social repercussions. The analysis of the results of this study, conducted on a sample of 40 patients in Cotonou, highlights significant aspects of this pathology, including the types of incontinence, associated dysfunctions and their impact on the quality of life of patients.
The results indicate that urinary incontinence due to neurological deficiencies is the most common, affecting 30% of patients in the context of bladder sphincter dysfunction. This is followed by incontinence related to trauma to the bladder sphincter (17.5%) and the urethra (12.50%). These results confirm the importance of neurological factors in the etiology of urinary incontinence in the elderly. Recent studies have shown that patients suffering from neurodegenerative diseases, such as multiple sclerosis or Parkinson’s disease, are particularly exposed to this type of dysfunction [14]. This link between neurological disorders and urinary incontinence underlines the need for specific and adapted management of these pathologies.
Ordinary urinary incontinence only affects 15% of cases, which corroborates the work of Irwin et al., who state that this type of incontinence is often underdiagnosed or minimized by patients themselves, due to the shame or taboo surrounding this problem [3]. However, nocturnal (10%) and daytime (5%) urinary incontinence also affects a significant proportion of the sample, showing that urinary disorders are not simply related to neurological deficiencies but can also be of behavioral or environmental origin.
The psychological impact of incontinence is considerable, as shown by the results of this study. Indeed, 15% of patients suffer from personality disorders, while 12.5% have behavioral disorders, including disturbed eating behaviors. These results are consistent with the studies of Felde et al., which showed that urinary incontinence, particularly in the elderly, causes a significant deterioration in self-esteem, which can lead to anxiety or depressive disorders [15]. This psychological suffering is often exacerbated by social isolation, as highlighted by Monz et al., as incontinent people tend to avoid social interactions for fear of an “accident” in public [16].
The results also reveal a notable prevalence of cognitive and psychotic disorders in these patients, at 5% and 25% respectively. Although this may seem high, these figures are consistent with the work of Farres-Godayol et al., who state that urinary incontinence is often associated with cognitive impairment, particularly in patients with dementia [17]. Indeed, these patients often lose the ability to recognize the physiological signals associated with urination, which worsens the impairment (Figure 1).
In addition, urinary incontinence causes somatic complaints, with 10% of patients suffering from psychosomatic complaints, such as insomnia and digestive disorders. These findings are supported by the research of Smith et al., who demonstrate that urinary incontinence can cause chronic pain, constipation and other somatic symptoms [8]. These physical and psychological consequences highlight the urgency of multidisciplinary management. It is also worth mentioning that this study highlights deficits in patient management. The coordination between the bladder and the sphincter, ensured by innervation, is often dysfunctional in these patients, with 55% of failures in the orthosympathetic system. This shows the importance of neuro-urological assessment to improve the management of incontinence. Indeed, treatments based on nerve stimulation can help restore this coordination in certain patients [18].
Finally, this study highlights the urgency of early and multidisciplinary intervention for these patients. Urinary incontinence in the elderly is not only a physical pathology, but it also deeply affects their psychological and social well-being. Early detection, adapted management strategies, including behavioral therapy, physiotherapy and psychological support, must be implemented to improve the quality of life of these patients [19].
Conclusion
Senior citizens face many challenges related to social difficulties and disorders of organic and psychological functioning. Sometimes, a person who already lives in a nauseating economic precariousness has chronic pathologies, transit or elimination disorders and mental disorders. This disease, being a source of organic suffering, is detrimental to their well-being. However, there is a social silence around the suffering of this social category. It is easy for relatives or specialists to say “in any case, he or she is old” when faced with suffering that should not normally be trivialized. Thus, we find ourselves in a context of trivialization of the suffering of senior citizens. Among the most common pathologies suffered by senior citizens is urinary incontinence, a serious urination disorder. It has a serious impact on all aspects of the life of the elderly person who, despite themselves, suffers from the quality of their life that is deteriorating. To analyze the impacts of this disorder on the psychological and social functioning of this disorder on this social category, we initiated this research. The results from the investigation allow us to remember that the suffering of the elderly in relation to urinary incontinence is cruel. We can also remember that there is a high proportion of elderly people who suffer from this organic disorder, strongly impacting psychological and social functioning. It should also be noted that in dependent elderly people, disorders of higher functions as well as loss of mobility, represent an important etiology of urinary incontinence. An elderly person presenting urinary incontinence (temporary or chronic) is therefore at risk of developing psychopathologies. These may be linked to their personality, their history and the history of their family. At the Centre National Hospitalier Universitaire Hubert Koutoukou MAGA (CNHU-HKM), the technical support platform is relatively limited. In the support protocol, there is an omission of psychological care, which should normally be at the top of this intervention process. Experience has shown that cognitive and behavioral therapies give satisfactory results in the treatment of psychological disorders concomitant with urinary incontinence. It is therefore urgent to improve the quality of the technical platform in terms of technicality for better orientation and management of voiding disorders. It is therefore important, even essential, that the state, the family, caregivers and the elderly person, prone to urination disorders, each as far as they are concerned, work to involve psychological support in the management of urinary incontinence and urination disorders with a view to better results for the health system in Benin according to the requirements of Sustainable Development Goal 3 (SDG 3).
References
- Abrams P, Cardozo L, Wagg A, Wein A. Incontinence (6th ed.). International Continence Society. 2017.
- Thüroff JW, Abrams P, Andersson KE, Artibani W, Chapple CR, et al. EAU guidelines on urinary incontinence. Eur Urol. 2011;35(7):373-388.
[Crossref][Google Scholar][PubMed]
- Irwin DE, Kopp ZS, Agatep B, Milsom I, Abrams P. Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int. 2011;108(7):1132-1138.
[Crossref][Google Scholar][PubMed]
- Monod S. How to screen geriatric conditions in primary care? Rev Med Suisse. 2009;5(224):2205-2206.
[Google Scholar][PubMed]
- Deffieux X. Urinary incontinence and pregnancy. J Gynecol Obstet Biol Reprod. 2009;38(8):S212-S231.
[Google Scholar][PubMed]
- Cahill J. Impact of Urinary Incontinence in Canada: A Policy Brief. Incontinence Foundation. 2009:25.
- National Institute of Statistics and Economic Analysis (INSAE) Demographic Survey. Cotonou. 2008.
- Smith PP, Dhaliwal G, Gormley EA. Chronic pelvic pain and urinary symptoms. J Urol. 2019;202(5):928-936.
- Boddaert J. Senior Citizens and Vulnerability Related to Communication Disorders. 2013.
- El Khoudri N. Urinary incontinence and well-being of older women. J Geriatr Urol. 2020;15(2):45-60.
- Bruno J, Lepetit P. Prevalence of mental disorders in incontinent elderly subjects. J Geriatr Psychiatry. 2015;8(3):1-15.
- Mareau S, Vanek-Dreyfus F. The psyche of the elderly and the impact of urinary disorders. J Geriatr Gerontol. 2010;5(4):200-215.
- Le Rouzo J. Psychotic disorders and aging: Cognitive fragility and loneliness. 2008.
- Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary incontinence in women: A review. JAMA. 2017;318(16):1592-1604.
[Google Scholar][PubMed]
- Felde G, Ebbesen MH, Hunskaar S. Anxiety and depression associated with urinary incontinence. A 10-year follow-up study from the Norwegian HUNT study (EPINCONT). Neurourol Urodyn. 2016;36:322.
[Crossref][Google Scholar][PubMed]
- Monz B, Pons ME, Hampel C, Hunskaar S, Quail D, et al. Patient-reported impact of urinary incontinence-results from treatment seeking women in 14 European countries. Maturitas. 2005;52:24-34.
[Crossref][Google Scholar][PubMed]
- Farrés-Godayol P, Jerez-Roig J, Minobes-Molina E, Yildirim M, Molas-Tuneu M, et al. Urinary incontinence and its association with physical and psycho-cognitive factors: a cross-sectional study in older people living in nursing homes. Int J Environ Res Public Health. 2022;19(3):1500.
[Crossref][Google Scholar][PubMed]
- Kessler TM, Fowler CJ, Panicker JN. Neurogenic lower urinary tract dysfunction in patients with multiple sclerosis. Nature Reviews Urology. 2016;13(5):275-288.
- Saussine C. Urinary Incontinence in Women. Progress in Urology, Elsevier Masson. 2009;19:279-284.
Citation: Psychological Implications of Urinary Problems in the Elderly at Cnhu-Hkm in Cotonou (Benin) ASEAN Journal of Psychiatry, Vol. 25 (8) October, 2024; 1-10.