Abstract
Objectives: The postpartum period is considered a time when mothers, living in stressful situations, are at higher risk of developing mental health issues. This could have long term health and well-being implications, in particular for women who experience postpartum depression who are more likely to develop depression later on in life. Aim: To assess the prevalence of postpartum depression following child birth and its relationship with social support and marital satisfaction. Study participants: A convenience sample of 185 postpartum women at approximately 10 weeks post-delivery was recruited to the study. The study was conducted at four Maternal and Child Health Centres, in KSA Methods: A descriptive correlational research design was used and data was collected on demographics, education level, parity, marital and estimates of experiencing depression symptoms using the Beck’s Inventory scale Results: The research findings comprised of varied qualitative and quantitative outcomes in relation to socio-demographics and mental health history. Conclusion: A significant proportion of mothers, in the early childbirth period, experience PPD and this are correlated with lower levels of social support and marital relation satisfaction. Nurse interventions could target these issues to help prevent mothers in the early childbirth period from experiencing episodes of depression.
Keywords
Postpartum, Postpartum Depression, Social Support, Marital Satisfaction, Women Health
Introduction
The postpartum period is a significant time for women since it is characterized by changes and challenges which if not effectively managed can increase the risk of developing physical and mental disorders [1]. It represents an essential life stage in which the accurate detection and treatment of psychological distress is important [1,2]. For example, the first week or month following giving birth can be characterized by elevated emotional imbalance. These emotions can be attributed to the fact that the mother is nursing their baby, while also adapting to disrupted sleeping patterns and recovering from the physical demands of childbirth. Furthermore,
the emotional imbalance can be associated with fatigue, hormonal changes, the pain of incisions, and swollen breasts or sore nipples. The postpartum period comprises of several changes in marital and family relations [3]. It may also be accompanied by financial burdens especially for individuals in lower social class. Research shows that 85% of women experience “slight depression or baby blues,” shortly after giving birth [4]. The slight depression is often accompanied by unexpected mood swings. However, the mood swings may be temporary and disappear after some time. If they persist, the depression can interfere with the mother’s daily activities
including their ability to concentrate and relate with other people. If untreated, the condition can last for up to one year. For that reason, patients should be evaluated for serious mood disorders after two weeks of slight depression following birth (WHO guideline).
Post-Partum Depression (PPD) is the most common type of severe mental disorder that has become a major public health concern. PPD is considered as one of the major depressive disorders that can be experienced at point of the first year of postpartum. Its peak is experienced in the first 4 months of the postpartum period. According to the Diagnostic and Statistical Manual of mental Disorder (DSM-IV), PPD is most likely to start around the four weeks period after birth [5]. On the other hand, the International Classification of Diseases (ICD) reports that PPD occurs within six weeks from childbirth. The ICD differentiates PPD from postpartum blues, which begin in the first or second week postpartum.
As demonstrated by many researchers, the prevalence of PPD globally is between 10% and 20% [6,7]. The World Health Organization (WHO) communicated that the occurrence of depression in the postpartum period is three times more likely at any other periods in a woman’s life. In Western countries, depression is the most common postnatal complication. Research shows that between 5% and 25% of mothers experience depressive episodes with the prevalence rates for socioeconomically disadvantaged groups higher at an approximated 38% [8-10]. For example, the prevalence of postpartum depression in Saudi Arabia is 23.9% [11]. The most common symptoms of PPD are feelings of hopelessness, inadequacy, gloominess, inability to feel joy with the baby, severe anxiety, loss of appetite, social isolation, suicidal thought, thoughts of harming the baby and sleep disturbance [12,13]. The postpartum period has negative effects on the mother herself as well as her children and family [14]. PPD affects the mother's quality of life and the functioning of her family and can have negative implications on the mental health of the child as well as their holistic growth and development [15,16].
Factors that can cause depression include physiologic, psychosocial, socio-demographic, genetic, and educational background. Besides, prematurity, low birth weight new-born, low incomes, antenatal depression, prenatal stressors, hormonal changes, prior episodes of postpartum depression, sleep deprivation, bipolar disorder, complications of pregnancy, delivery, and after birth, postnatal anxiety, a family history of depression, unplanned pregnancy, perceived social support, and lack of marital satisfaction [17-20].
Several researchers [21-23] indicate that inadequate perceived social support is a major contributing factor to PPD. Social support is the accessibility and availability of help from people when it is needed. Perceived social support is the backup from family members, friends, colleagues, neighbours, professional people, and organizations when help is needed the most. On the other hand, lack of social support accompanied with dissatisfaction and problems in marital relationships and financial limitations can lead to severe stress causing PPD. The relationship between marital satisfaction, parental anxiety and PPD has been reported by many researchers.
Perceived social support is a satisfaction with informal individuals and groups such as a partner, friends, family, and loved ones. It is also considered a satisfaction with formal groups and individuals such as general practitioner, midwife, and other health care professionals. These social relations are frequently associated with positive health outcomes especially for mothers suffering from PPD. The relationship is distinguishable from informal social support which is the cumulative supportive behaviours that enhance better outcomes during the postpartum period. In addition, lack of social support during pregnancy is regularly associated with a higher risk of PPD [24-26].
In the postnatal period, the mother requires a lot of attention and support. Due to the criticalities of these demands, parents cope with the newborn situation. In most cases, the parents are forced to adapt economic and social impact brought about by the infant. The situation can be highly-demanding such that emotional instabilities can be triggered.
Marital satisfaction is defined as the subjective experience of contentment and happiness in a marital relationship. From a therapeutic perspective, marital satisfaction has a psychological wellbeing that enlivens the postnatal period. For example, the marital satisfaction can be brought about by the husband’s love, helpful attitude, and attention during pregnancy and the postpartum period. The support from the husband also incorporates verbal and nonverbal supportive communication to facilitate the wife’s decision-making and comforts [27].
Prevention of PPD is therefore of highest priority in light of the high morbidity associated with the condition. For that reason, it is recommended that a maternity nurse should screen high-risk mothers for PPD. This is crucial before and after childbirth. The results of the screening process identifying risk of PPD, should be referred to the community mental health centres for early management and prevention of mental health issues. Additionally, health care authorities should develop strategies to design recommendations and actions to prevent PPD [27-29].
Significance of the Study
Since PPD is perceived as a mental health problem, its relationship with social support and marital satisfaction has increased a lot of research on the field. The outcomes of the research are urgently needed by practitioners such as nurses and other researchers. Understanding the impact of social support and marital satisfaction has important implications for preventing and managing PPD. Prevention of PPD is essential for mothers' wellbeing and provides a conductive atmosphere for the new-born. Thus, this study aim is to assess the relationship between postpartum depression and social support and marital satisfaction.
Aim of the Study
This study aimed to assess prevalence of PPD and any correlation between postpartum depression, history of mental health issues, social support and marital satisfaction.
Research Questions
• What is the prevalence and severity of PPD in the early post-delivery period.
• Are there significant associations between levels of social support and marital satisfaction and developing postpartum depression.
Materials and Methods
Research design
The current study used a descriptive correlational research design.
Research setting
The current study was conducted at four maternal and child health centres affiliated to the Ministry of Health in Makah and Riyadh cities:
• The current study was conducted at obstetric and outpatient clinics in three selected general hospitals: two at Makkah al-Mukaramah city and one in Riyad city in Saudi Arabia; these hospitals are affiliated with the Ministry of health.
• One other psychiatric and mental health hospital (at outpatient mental health clinic) in Riyadh City in Kingdom of Saudi Arabia is affiliated with the Ministry of health.
Research subjects
A convenient sample of 185 postpartum women at approximately 10 weeks post-delivery. In the research, women were selected from the maternal and child health centres who came for receiving postpartum follow-up or taking their baby for immunizations.
85 women from the mental hospital outpatient clinics who already diagnosed with PPD were recruited in the study according to the following criteria:
Inclusion criteria
• Married, age ranged from 20 to 40 years old.
• Able to read and
• Have a healthy single full-term
• No complications during pregnancy, childbirth, and
Beck Depression Inventory was applied for total study women. Based on women reported scores,
(32) women of one hundred who not diagnosed PPD had a score of 10 or greater these women were added to the 85 women who diagnosed with PPD became 117 women. Whereas the rest (68) women who reported scores less than a score of 10 considered normal (without PPD) group.
Tools of Data Collection
The tools that were used for data collection include:
A Self-Administered Questionnaire
This tool has the following two parts:
• Socio-demographic characteristics: such as mothers' age, level of education, family income and work
• Obstetric history: It concerned with data regarding gravidity, parity, previous abortion, type of delivery, new-born gender, number of children, history of postpartum depression, mental illness and prenatal
Beck Depression Inventory (BDI)
BDI is used to determine the levels of depression among patients based on the descriptions of their symptoms. The tool has 21 self-reports based on a four-point Likert scale score that ranges from 0 (no symptoms) to 3 (very intense symptoms). Based on the BDI tool scores a total of between 0 and 9 is considered normal. A score that ranges between 10 and 18 is mild, while a score between 19 and 29 is considered moderate. On the extreme end, a total score between 30 and 63 implies severe depression. From that classification, it is evident that higher total scores indicate severe depressive symptoms [30,31]. On the other hand, a total score above. High concurrent validity ratings are assigned between the BDI and other depression scales. For example, 0.77, and its reliability is 0.96 (Alfa- coefficient).
Multidimensional Scale of Perceived Social Support (MSPSS)
MSPSS tool has the benefit of being free of social desirability bias. The MSPSS tool had 12-items. The tool was used to assess three sources of support including friends support, family support, and significant others support. The participants using the MSPSS are required to indicate their agreement that is represented on a 5-point Likert - type structure. In the Likert scale, 1 means “strongly disagree” and 5 implies “strongly agree.” The tool was modified from a 7 point Likert-type to since the differences between adjacent categories is minor. After the modification, the scale became easier for the participants to respond by subjects. The internal consistencies of the Cronbach's alpha (subscales) are 0.76, 0.78 and 0.70 for friends support, family support, and significant other support, respectively. The highest mean score represents outstanding social support [32,33]
Couples Satisfaction Index (CSI)
The tool was designed to measure an individual’s satisfaction in a marital relationship. The CSI scale was composed of 16 items. The items of CSI are rated on a 6-point response that ranges from “never” to “all the time.” The tool demonstrated significant internal consistency, with a standardized Cranach’s alpha of "0.92".
The maximum score is "93" a score of "55" equal ≥ 60% equal consider high marital relation satisfaction, from "54-41" equal ≤ 60% is deemed to be moderate, while "40-27" equal ≤ 50%-33% mild and while a score of "27 or less " equal ≤ 33% has been validated to identify relationship distress.
The third and fourth scales were translated to the Arabic language by the investigators, and back translation to the English language was performed as a validity check. Five experts in the obstetric and psychiatric nursing fields tested its validity.
Study Preparation
• Review of the past and current related literature covering all aspect of the problem using available books, journals, articles, and magazines was done to get acquainted with research problem and develop the study
• An approval from ethical committee, Faculty of Nursing- Umm Al-Qura University was
• An official letter from the Faculty of Nursing, Umm Al-Qura University was obtained and directed to the responsible authorities at the study settings for permission to conduct the
• A pilot study was conducted at the beginning of the study. It included 10% of the study sample (18 women in the previously mentioned settings) to investigate the feasibility of data collection tools, their clarity, and the time required to fill the tools. Results of the pilot study did not lead to any modifications of questions. Subjects included in the pilot study were excluded from the total studied
Ethical Consideration
All the relevant ethical principles in the research were followed. The Institutional Research Board reviewed the study protocol and study approval received. Participant’s informed consent to participate was obtained after informing them about their rights to participate, refuse, or withdraw at any time without any detriment to their care. Total confidentiality of any received information was ensured. The study manoeuvre could not entail any harmful effects on participants. Data protection and security was ensured through use of password controlled computerized databases.
Data Collection
Data were collected in the period from the beginning of May to the end of December 2017. The researchers were available 2 days/week at the previously selected health settings from 8 am-12 pm. The researchers introduced themselves and provided explanations to mothers who met the study criteria about the study's nature, aim, and purpose. Each woman was informed that sharing in this study is voluntary. Verbal approval of women to participate in this study was achieved. Mothers were interviewed individually in a private room in the study settings. Each interview lasted about 25-45 minutes. In the end, the researchers thanked all interviewed women.
Data entry and statistical analysis were done using SPSS 20.0 statistical software package. Data were presented using descriptive statistics, and comparison between groups was done by using Chi-square and T-test. Pearson Correlation analysis was used to identify the inter- relationships between variables. Statistical significance was considered at a p-value ≤ of 0.05.
Results
Table 1: Distribution of the mothers according to socio-demographic data (n=185)
| Items |
Total N=185 |
| No. |
% |
| Mother age (year) |
|
|
| 20-25 years |
52 |
28.1 |
| 25-30 years |
60 |
32.4 |
| 30-35 years |
48 |
25.9 |
| 35-40 years |
25 |
13.5 |
| Mean ± SD 28.7 ± 4.6 |
| Mothers'educational level |
|
|
| Read and write |
14 |
7.6 |
| Preparatory |
24 |
13 |
| Secondary |
52 |
28.1 |
| University |
95 |
51.3 |
| Working state |
|
|
| Working |
68 |
36.8 |
| Housewives |
117 |
63.2 |
| Family income |
|
|
| Sufficient |
166 |
89.7 |
| Insufficient |
19 |
10.3 |
| Number ofchildren |
|
|
| 0-3 |
84 |
45.4 |
| 3-5 |
72 |
38.9 |
| ≥ 6 |
29 |
15.7 |
Table 1 show that nearly one-third of the mothers (32.4%) aged between 25 to 30 years, while 13.5% were between 35-40 years old with a mean age of 28.7 ± 4.6. Regarding the educational level, slightly more than half of the subjects (51.3%) had university education, while only • % can read and write. Besides, about two- thirds of mothers (63.2%) were housewives. Also, the majority (89.7%) have sufficient income. More than one-third of women (38.9%) had 3-5 children.
Table 2: Distribution of the mothers according to their obstetric history (n=185)
| Items |
Without depression |
With depression |
X2 |
| (N=68) |
(N=117) |
p-value |
| No. |
% |
No. |
% |
| Type of delivery |
| Spontaneous vaginal delivery |
33 |
48.5 |
84 |
71.8 |
6.4 |
| Caesarian suction |
35 |
51.5 |
33 |
28.2 |
0.01** |
| Infant gender |
| Boy |
29 |
42.6 |
72 |
61.5 |
9.8 |
| Girl |
39 |
57.4 |
45 |
38.5 |
0.00** |
| Gravidity |
| Once |
31 |
45.6 |
26 |
22.2 |
13.7 |
| Twice |
10 |
14.7 |
20 |
17.1 |
0.00** |
| Three or more |
27 |
39.7 |
71 |
60.7 |
| Presence of abortion |
| Never |
46 |
67.7 |
65 |
55.6 |
4.38 |
| 1 |
13 |
19.1 |
30 |
25.6 |
| ≥ 2 |
9 |
13.2 |
22 |
18.8 |
0.32 |
**: Correlation is significant ≤ 0.01 level
Table 2 illustrates that 71.8% of women with PPD had Spontaneous vaginal delivery than 48.5% of mothers without PPD. Also, 61.5% of mothers who gave birth to a male infant suffered from PPD, compared to 42.6% of mothers without PPD with female baby. The difference is statistically significant between the two groups (p=0.00). The gravidity of 60.7% of mothers who suffered from PPD was three or more than 39.7% of mothers without PPD; the difference is statistically significant (p=0.00).
Table 3: Distribution of mothers according to their family history of mental illness and history of PPD (n=185)
| Items |
Without depression |
With depression |
X2 |
| (N= 68) |
(N= 117) |
p-value |
| No. |
% |
No. |
% |
| Family history of mental illness |
| Yes |
5 |
7.4 |
76 |
65 |
16.32 |
| No |
63 |
92.6 |
41 |
35 |
0.00** |
| PPD Starting during pregnancy |
| Yes |
6 |
8.8 |
70 |
59.8 |
47.2 |
| No |
62 |
91.2 |
47 |
40.2 |
0.00** |
| Previous PPD history |
| Yes |
16 |
23.5 |
103 |
88 |
74.73 |
| No |
52 |
76.5 |
14 |
12 |
0.00** |
**: Correlation is significant ≤ 0.01 level
Table 3 reveals that postpartum depression started from pregnancy in 59.8% of women. Most of the mothers (88.1%) who suffered from PPD had a previous history of PPD (Table 3). However, there was a statistically significant difference between the two groups regarding family history, starting the depression during pregnancy, and history for PPD, respectively (P=0.00).
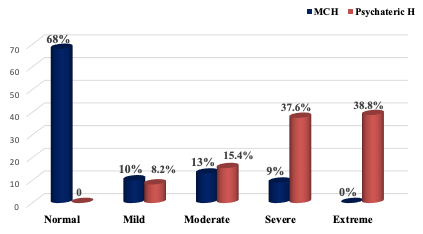
Figure 1 indicates that 63% of mothers interviewed at Maternal and child health centres were not suffering from PPD; assessed as "normal" according to Beck Depression Inventory. 10% and 13% of mothers suffered from mild and moderate depression levels, respectively, while only 9% of mothers suffered from severe depression. As for mothers diagnosed with PPD, only 8.2% suffered from mild depression, 15.4% suffered from moderate depression. However, more than one-third (37.6%) and (38.8%) of mothers suffered from severe and extreme depression, respectively.
Table 4: Mean scores differences of social support scale and its' subscales according to mothers' depression levels (n=185)
| Subscale items |
Depression level |
F- test |
P-value |
| Normal "68" |
Mild "17" |
Moderate"28" |
Severe ''41'' |
| Family support |
17.51 ± 3.02 |
16.75 ± 2.33 |
9.28 ± 3.58 |
5.37 ± 4.11 |
72.4 |
0.00 |
| Friend support |
16.13 ± 3.60 |
14.76 ± 2.84 |
13.63 ± 3.91 |
8.27 ± 3.52 |
58.5 |
0.00 |
| Significant other |
15.75 ± 5.15 |
14.29 ± 4.26 |
10.60 ± 5.66 |
8.35 ± 4.16 |
28.0 |
0.00 |
| Total support |
49.27 ± 9.03 |
45.88 ± 7.01 |
38.76 ± 1.76 |
26.88 ±7.62 |
63.58 |
0.01 |
**: Correlation is significant ≤ 0.01 level
Table 4 depicts that the highest mean scores of "49.27 ± 9.03" for total social support and its' subscales; family, friends and significant others support "17.51 ± 3.02", "16.13 ± 3.60" and "15.75 ± 5.15" respectively were reported by women who had not suffered from PPD. It can also be noted that the intensity of PPD increased as the mean score of total social support and its' subscales declined. There are significant differences between mean scores of comprehensive social support, family support, friend support, and substantial other support correlated with PPD levels, p ≤ 0.01 levels.
Table 5: Relationship between mothers' depression levels and couples satisfaction index (n=185)
| Couple satisfaction levels |
Depression level |
| Normal "68" |
Normal "68" |
Normal "68" |
Normal "68" |
Normal "68" |
| No. |
% |
No. |
% |
No. |
% |
No. |
% |
No. |
% |
| High (55-80) |
45 |
71.4 |
9 |
52.9 |
7 |
22.6 |
2 |
4.9 |
0.0 |
0.0 |
| Moderate( 53-28) |
18 |
28.6 |
8 |
47.1 |
18 |
58.1 |
18 |
43.9 |
9 |
24.2 |
| Low or distress(≤ 27) |
0 |
0.0 |
0 |
0.0 |
6 |
19.3 |
21 |
51.2 |
25 |
75.8 |
| Chi-Square test P value |
112.370.00** |
**: Correlation is significant ≤ 0.01 level
Table 5 shows that there are statistically significant differences between PPD level and couple satisfaction level (P=0.00). About three- quarters of mothers, 71.4% had high couple
satisfaction did not suffer from PPD. Additionally, 51.2% and 75.8% of mothers who have couple relation distress suffered from severe and extreme depression levels.
Table 6: Coefficient correlation between postpartum depression and both of social support and couple satisfaction (n= 85)
| Variables |
Pearson correlation |
Couple satisfaction |
Depression |
| Depression |
R |
-0.785 |
- |
| P-value |
0.00** |
0.00** |
| Family support |
R |
0.695 |
-0.707 |
| P-value |
0.00** |
0.00** |
| Friend support |
R |
0.637 |
-0.648 |
| P-value |
0.00** |
0.00** |
| Significant others support |
R |
0.526 |
-0.532 |
| P-value |
0.00** |
0.00** |
| Total Social support |
R |
0.717 |
-0.737 |
| P-value |
0.00** |
0.00** |
**: Correlation is significant ≤ 0.01 level
Table 6 Shows that there is a statistically significant strong negative association between PPD and total social support and its' subscales; family, friend, and significant others support (R=- 0.737), (R=-0.707), (R=-0.648) and (R=-0.532).
Additionally, there was a statistically significant strong negative association between post-partum depression and couple satisfaction (R=-0.785) p values for all variables p=0.00.
Discussion
The study aim was to assess the relationship between postpartum depression and social support and marital satisfaction and found a significant proportion of mothers, in the early childbirth period, experience PPD and this is correlated with lower levels of social support and marital relation satisfaction. The prevalence of PPD varies significantly depending on the description of the disorder, country, diagnostic tools used, and period that the prevalence is determined, and the threshold of discrimination chosen for the screening measure. Nevertheless, the prevalence of PPD in Saudi Arabia in Saudi study was 23.9% [34]. Moreover, the prevalence of PPD in Egypt is estimated between 10% and 20%, with an average prevalence of 13% [35]. In developing countries, the prevalence has been determined to range between 5.2% and 74.0%, with the highest prevalence reported in Turkey and lowest prevalence in Pakistan.
The significant variation in the prevalence of PPD can be attributed to the use of different diagnostic tools as well as a heterogeneous study designs. For example, the research used tools such as the EPDS, MSPSS, BDI, and CSI [36]. As demonstrated by the outcomes of the research, the prevalence of PPD was 33.3%. On the other hand, marital dissatisfaction was reported to be 39.5% of 22 mothers (participants). Additionally, 22.0% had co-morbid depression and anxiety as well as worse marital dissatisfaction.
In the meta-analyses and systematic reviews used for the research, six health-related databases were selected. The databases included Medline, SCOPUS, Informit, psych info, Cinhal. Furthermore, the research used Cochrane systematic reviews for the prevalence and the correlations factors of depression in Australian women. The results showed 2.6% to 43.9% prevalence rates of depression among women. However, the prevalence rates differ from one region to another. The disparities can be attributed to the socioeconomic status and other social determinants of health [37]. PPD is considered one of the global rising epidemics. For example, the current global show between 11% and 42% of PPD among women globally.
These findings supported the current study findings that 32% of the study women in 2: 20 weeks after delivery and come for following up in general hospitals either paediatric or obstetric clinics suffered from PPD. Highlighting the study women's nearly two-thirds of the study women in the age group of 20 to 30 years were not working even though about half of them had a university education. This may affect women's life quality [38].
Regarding the relationship between PPD and infant sex. Research shows that women who give birth to a male infant were related to less PPD. Additionally, the women who give birth to a female infant reported inadequate or insufficient postpartum support from family members particularly husband and parents. This finding is inconsistent with the present study results as nearly two-thirds of women who give male infants after birth suffered from PPD compared with 38.9% of women who gave female infants. The findings show multiple logistic regression model that was having a male infant was a risk factor for mothers’ severe distress, thereby at higher risk for occurrence of PPD. Also, postnatal family support scores were much lower in women who gave birth to a female infant than women who gave birth to a male infant [39].
Focusing on the results of investigating the correlation between social supports and developing the PPD, proved that both teen and adult mothers were about five times likelier to experience PPD. This is evident if they did not receive support or minimal support after the birth of a baby. Furthermore, research shows that that social support during prepartum and postpartum periods has significant implications on depression. For example, women with both prepartum and postpartum depression had fewer supportive people around them and had lower levels of marital satisfaction [40]. These findings supported current study findings; the highest mean scores of social support, “family, friends, and the significant others,” were reported by women who did not suffer from PPD. The mean
scores were significantly declined among women who are suffering from worse levels of PPD. Additionally, a statistically significant negative association was found between social support and the development of PPD [41]. This explains the current study findings that a statistically strong negative significant association between PPD among the study women was interviewed 2- 16 weeks post-delivery and their scores for couple satisfaction [42,43].
Conclusion
The outcomes of the study show that lack of social support, poor marital adjustment can lead to depression in women following childbirth. The current study findings postulate that there is a significant relationship between PPD and marital satisfaction level. Women who had couple relation distress are mostly suffering from PPD than women with moderate or high couple satisfactions. Conversely women with high couple satisfaction were not suffering from PPD. This finding shows that lack of their husbands' support is a significant risk factor of PPD.
As demonstrated by the findings of the research, it is evident that there is a significant and inverse correlation between marital satisfaction and PPD. Additionally, research shows that couples with effective marital communication and understanding enjoy a better health status. Additionally, women who reported higher levels of social support had fewer symptoms of depression during the postpartum period in comparison to women with less supportive networks. From clinical application, practical PPD intervention approaches should incorporate amenable factors. However, the type and timing of the intervention are still clearly outlined.
References
- Nurbaeti I, Deoisres W, Hengudomsub P. Association between psychosocial factors and postpartum depression in South Jakarta, Indonesia. Sexual Reproductive Healthcare. 2019; 20: 72-6.
- 2. Odinka JI, Nwoke M, Chukwuorji JC, Egbuagu K, Mefoh P, Odinka PC, et al. Post-partum depression, anxiety and marital satisfaction: A perspective from Southeastern Nigeria. South African Journal of Psychiatry. 2018; 24.
- Nurbaeti I, Deoisres W, Hengudomsub P. Association between psychosocial factors and postpartum depression in South Jakarta, Indonesia. Sexual Reproductive Healthcare. 2019; 20: 72-6.
- Chaput KH, Nettel A, Musto R, Adair CE, Tough SC. Breastfeeding difficulties and supports and risk of postpartum depression in a cohort of women who have given birth in Calgary: A prospective cohort study. CMAJ open. 2016; 4(1): E103.
- Ohara MW, McCabe JE. Postpartum depression: current status and future directions. Annual review of clinical psychology. 2013; 9: 379-407.
- Werner E, Miller M, Osborne LM, Kuzava S, Monk C. Preventing postpartum depression: Review and recommendations. Archives of women's mental health. 2015; 18(1): 41-60.
- Bérard A, Abbas F, Kassai B, Vial T, Nguyen KA, Sheehy O, et al. The French Pregnancy Cohort: Medication use during pregnancy in the French population. PloS One. 2019; 14(7): e0219095.
- Shorey S, Chee CY, Ng ED, Chan YH, San Tam WW, Chong YS, et al. Prevalence and incidence of postpartum depression among healthy mothers: a systematic review and meta-analysis. Journal of Psychiatric Research. 2018; 104: 235-48.
- O'hara MW, McCabe JE. Postpartum depression: current status and future directions. Annual Review of Clinical Psychology. 2013; 9: 379-407.
- Almarzouki AM, Alzaben F, Sawan D, Filimban R. The prevalence of post-partum depression and its associated risk factors in Jeddah, Saudi Arabia: An observational study. Life Science Journal. 2015; 12(12): 79-85.
- Meena PS, Soni R, Jain M, Jilowa CS. Cognitive dysfunction and associated behaviour problems in postpartum women: a study from North India. East Asian Archives of Psychiatry. 2016; 26(3): 104.
- depression. Current Opinion in Psychiatry. 2015; 28 (6): 490-6.
- Nurbaeti I, Deoisres W, Hengudomsub P. Association between psychosocial factors and postpartum depression in South Jakarta, Indonesia. Sexual Reproductive Healthcare. 2019; 20: 72-6.
- Shorey S, Chee CY, Ng ED, Chan YH, San Tam WW, Chong YS, et al. Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. Journal of Psychiatric Research. 2018; 104: 235-48.
- Odinka JI, Nwoke M, Chukwuorji JC, Egbuagu K, Mefoh P, Odinka PC, et al. Post-partum depression, anxiety and marital satisfaction: A perspective from Southeastern Nigeria. South African Journal of Psychiatry. 2018; 24.
- Biaggi A, Conroy S, Pawlby S, Pariante CM. Identifying the women at risk of antenatal anxiety and depression: a systematic review. Journal of Affective Disorders. 2016; 191: 62-77.
- Cankaya S. The effect of psychosocial risk factors on postpartum depression in antenatal period: A prospective study. Archives of Psychiatric Nursing. 2020; 34(3): 176-83.
- Munaf S, Siddiqui B. Relationship of post-natal depression with life and marital satisfaction and its comparison in joint and nuclear family system. Procedia-Social and Behavioral Sciences. 2013; 84: 733-8.
- Nurbaeti I, Deoisres W, Hengudomsub P. Postpartum depression in Indonesian mothers: its changes and predicting factors. Pacific Rim International Journal of Nursing Research. 2018; 22(2): 93- 105.
- Pow J, King DB, Stephenson E, DeLongis A. Does social support buffer the effects of occupational stress on sleep quality among paramedics. A daily diary study. Journal of Occupational Health Psychology. 2017; 22(1): 71.
- Bucholz EM, Strait K, Dreyer RP, Geda M, Spatz ES, Bueno H, et al. Effect of low perceived social support on health outcomes in young patients with acute myocardial infarction: results from the variation in recovery: Role of gender on outcomes of young AMI patients (VIRGO) study. Journal of the American Heart Association 2014; 3(5): e001252.
- Leung J, Pachana NA, McLaughlin D. Social support and health related quality of life in women with breast cancer: a longitudinal study. Psycho Oncology. 2014; 23(9): 1014-20.
- Milgrom J, Hirshler Y, Reece J, Holt C, Gemmill AW. Social support a protective factor for depressed perinatal women. International Journal of Environmental Research and Public Health. 2019; 16(8): 1426.
- Melrose KL, Brown GD, Wood AM. When is received social support related to perceived support and well-being when it is needed. Personality and Individual Differences. 2015; 77: 97-105.
- Ohara MW, McCabe JE. Postpartum depression: current status and future directions. Annual Review of Clinical Psychology. 2013; 9: 379-407.
- Munaf S, Siddiqui B. Relationship of post- natal depression with life and marital satisfaction and its comparison in joint and nuclear family system. Procedia-Social and Behavioral Sciences. 2013; 84: 733-8.
- Hynan MT, Steinberg Z, Baker L, Cicco R, Geller PA, Lassen S, et al. Recommendations for mental health professionals in the NICU. Journal of Perinatology. 2015; 35(1): 14-8.
- Johnson JE, Wiltsey S, Sikorskii A, Miller T, King A, Blume JL, et al. Protocol for the ROSE sustainment (ROSES) study, a sequential multiple assignment randomized trial to determine the minimum necessary intervention to maintain a postpartum depression prevention program in prenatal clinics serving low-income women. Implementation Science, 2018; 13(1): 1-12.
- Ruyak SL, Qeadan F. Use of the Antenatal Risk Questionnaire to Assess Psychosocial Risk Factors Associated with Risk for Postpartum Depression: A Pilot Study. Journal of Midwifery Women's Health. 2018; 63(5): 578-83.
- Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. Journal of Personality Assessment. 1988; 52(1): 30- 41.
- Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988; 8(1): 77-100.
- Mitchell J, Zimet GD. Psychometric properties of the Multidimensional Scale of Perceived Social Support in urban adolescents. American Journal of Community Psychology. 2000; 28(3): 391-400.
- Almarzouki AM, Alzaben F, Sawan D, Filimban R. The prevalence of postpartum depression and its associated risk factors in Jeddah, Saudi Arabia: An observational study. Life Science Journal. 2015; 12(12): 79-85.
- Funk JL, Rogge RD. Testing the ruler with item response theory: increasing precision of measurement for relationship satisfaction with the Couples Satisfaction Index. Journal of Family Psychology. 2007; 21(4): 572.
- Ohara MW, McCabe JE. Postpartum depression: current status and future directions. Annual Review of Clinical Psychology. 2013; 9: 379-407.
- Motzfeldt I, Andreasen S, Lynge A, Lynge M. Prevalence of postpartum depression in Nuuk, Greenland–a cross- sectional study using Edinburgh Postnatal Depression Scale. International Journal of Circumpolar Health. 2013; 72(1): 21114.
- Saxena S, Funk M, Chisholm D. WHO's mental health action plan 2013-2020: What can psychiatrists do to facilitate its implementation. World Psychiatry. 2014; 13(2): 107.
- Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988; 8(1): 77-100.
- American Psychiatric Association. DSM- IV: Diagnostic and statistical manual of mental disorders. 2015.
- Mughal S, Azhar Y, Siddiqui W. Postpartum depression. Stat Pearls. 2020.
- Biaggi A, Conroy S, Pawlby S, Pariante CM. Identifying the women at risk of antenatal anxiety and depression: a systematic review. Journal of Affective Disorders. 2016; 191: 62-77.
- Vaezi A, Soojoodi F, Banihashemi AT, Nojomi M. The association between social support and postpartum depression in women: A cross sectional study. Women and Birth. 2019; 32(2): e238-42.
- González G, Moraes M, Sosa C, Umpierrez E, Duarte M, Cal J, et al. Maternal postnatal depression and its impact on child neurodevelopment: A cohort study. 2017; 88: 360-6.