LORAZEPAM FOR THE MANAGEMENT OF POSTERIOR FOSSA MUTISM: A CASE REPORT
1Department of Psychiatry, King Abdulaziz University, Jeddah, Saudi Arabia
2Department of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia
3Department of Neurosurgery, King Abdulaziz University, Jeddah, Saudi Arabia
4Department of Neurosurgery, King Abdullah Medical City in Holy Capital, Makkah, Saudi Arabia
*Corresponding Author:
Sulhi Alfakeh, Department of Psychiatry, King Abdulaziz University,
Jeddah,
Saudi Arabia,
Email: salfakeh@kau.edu.sa
Received: 30-Apr-2024, Manuscript No. AJOPY-24-133610;
Editor assigned: 03-May-2024, Pre QC No. AJOPY-24-133610 (PQ);
Reviewed: 17-May-2024, QC No. AJOPY-24-133610;
Revised: 24-May-2024, Manuscript No. AJOPY-24-133610 (R);
Published:
31-May-2024, DOI: 10.54615/2231-7805.47352
Abstract
Posterior Fossa Syndrome (PFS) is a condition that can develop in children and adults
following a cerebellar tumor resection surgery. The syndrome is characterized by multiple
symptoms, including mutism, personality changes, and mobility problems. We present a case
of a four-year-old boy diagnosed with posterior fossa tumor with secondary hydrocephalus
who underwent an uneventful total resection of the tumor and developed posterior fossa
syndrome, including mutism, was managed using lorazepam and made a full recovery of
almost all of the symptoms he developed. Posterior fossa syndrome has multiple symptoms,
most of which are usually transient. The exact pathophysiology and time to recovery are
still not fully known. Patients with posterior fossa syndrome are managed with a multi-
disciplinary approach. Mutism resulting from this syndrome is proven to be successfully managed by lorazepam.
Keywords
Posterior Fossa Syndrome; Mutism; Cerebellar Mutism; Cerebellar Mutism
Syndrome; Lorazepam; Ependymoma; Pediatrics
Introduction
Posterior Fossa Syndrome (PFS) is a syndrome that
affects children and adults following a cerebellar
tumor resection surgery. It is a rare syndrome
that mostly affects children but can also occur in
adults. It is also known as posterior fossa mutism
syndrome and cerebellar mutism syndrome. The
syndrome is characterized by mutism, apraxia as
well as behavioral and personality changes. Other
reported complications commonly associated with
cerebellar surgery are cranial nerve palsies and
other neuropsychiatric symptom [1]. Patient that
experience symptoms of this syndrome usually
return to their preoperative state of health with
the proper management. The duration and severity
of symptoms varies form a patient to another but
it has been reported to be in the range of weeks,
months or even years [2].
The treatment of posterior fossa mutism syndrome
consists of both behavioral and biological modalities. Few studies have been done on the
rare complication of posterior fossa syndrome.
A study by Catsman-Berrevoets and Aarsen was
done in 2010. They reported 148 patients with
cerebellar tumor that underwent resection surgery.
They found that out of the 148 patients, 41 has
developed posterior fossa syndrome [1].
A case report was published in 2016 by Gadgil et
al., about a two year old girl with medulloblastoma
who underwent a resection of the tumor with
a posterior fossa craniotomy [3]. The patient
showed mutism but she showed improvement in
her mutism by a month following the surgery.
She was followed 45 months later and was found
to still have dysarthria despite having speech
therapy. Another case was also reported that
shows a two year old boy who was diagnosed
with an ependymoma. The patient underwent a
total resection by a posterior fossa craniotomy as
well. The patient developed mutism that resolved
completely 6 months following the surgery [3].
A more recent study was also done in 2021
which included 178 patients who were diagnosed
with medulloblastoma and underwent surgical
resection. It was found that 60 of them had
developed posterior fossa syndrome. Complete
mutism was found in forty of these sixty patients
affected while twenty patients had reduced speech
only. For those who experienced complete mutism,
the median time for full resolution of mutism
was 2.3 months. There were no pharmacological
protocols for management for post operation
complications including mutism. All those affected
would undergo behavioral and speech therapy [4].
Very few numbers of studies has been done on
the management of posterior fossa syndrome with
lorazepam. A case report that presents a 10 year
old boy who developed posterior fossa mutism
and was managed with lorazepam on an as needed
bases. His symptoms improved and he gained
speech back soon after [5].
In this case report we present a patient who was
diagnosed with posterior fossa mutism and was
treated successfully with lorazepam.
Case Presentation
A four year old presented to the emergency
department with a history of persistent vomiting
for twenty days, associated with headache,
photophobia, irritability, bilateral lower limb
weakness and significant weight loss.
The patient was admitted in the Pediatric Intensive
Care Unit (PICU) and Computed Tomography
(CT) brain was done which revealed posterior
fossa mass with hydrocephalus, and emergency
External Ventricular Drain (EVD) was inserted.
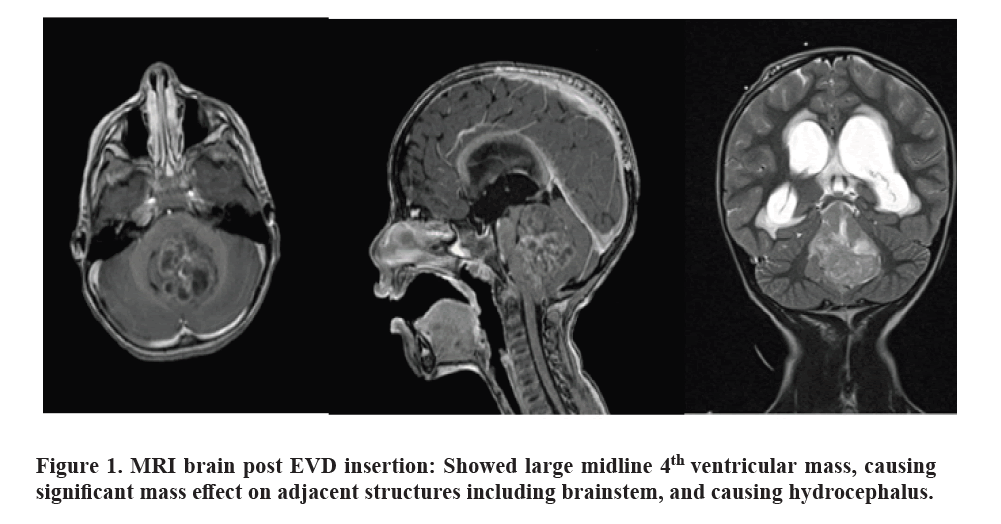
Magnetic Resonance Imaging (MRI) with contrast
was later performed, which showed large midline
posterior fossa mass that seems to be filling the 4th ventricle and extending through the foramen of
Luschka, with significant mass effect on Brainstem
and cerebellum. MRI whole spine showed no drop
metastasis.
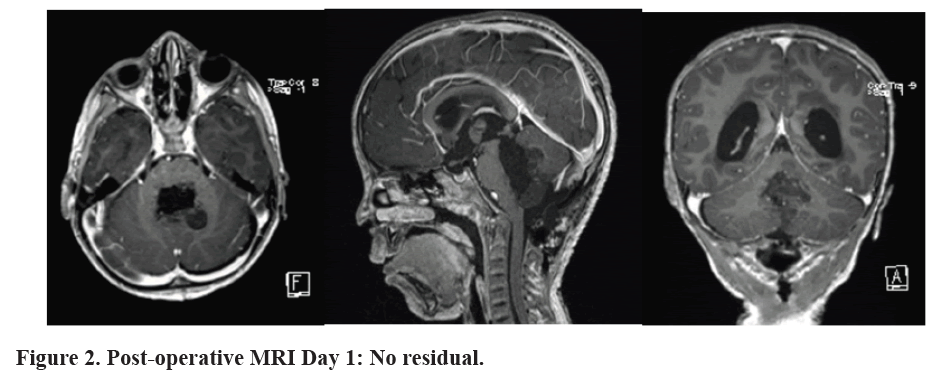
He then underwent a posterior fossa craniotomy
and gross total resection of the tumor, which
was successful and uneventful. The patient was
extubated after MRI brain with contrast was
done which showed complete resection and no
residual, post-operative examination patient
found to have right sixth and seventh nerve palsies
(facial collicular syndrome), he was also found to be mute, with personality changes, aggression
and decreased mobility. Histopathology report
was anaplastic ependymoma World Health
Organization (WHO) grade III.
Regarding behavior changes, aggression
and mutism; psychiatry were involved in the
multidisciplinary team managing the patient.
Patient was treated with low dose lorazepam and
was followed up both during admission and as in
outpatients setting. He was initially started on 0.25
mg of lorazepam twice daily but showed almost
no improvement. His dose was then increased to
0.5 mg twice daily and that’s when he started to
show improvement. He did not show any side
effects which made the increase in dose possible.
His dose was finally increased to 1 mg twice
daily and that’s when he showed rapid and major
improvements. His behavior improved as he
became calmer, he started smiling and was able
to play with his toys. Patient was able to start gain
back his speech abilities soon after the operation
and by his two months follow up he was able to
speak in words clearly. His behavioral symptoms,
aggression and mobility started to improve
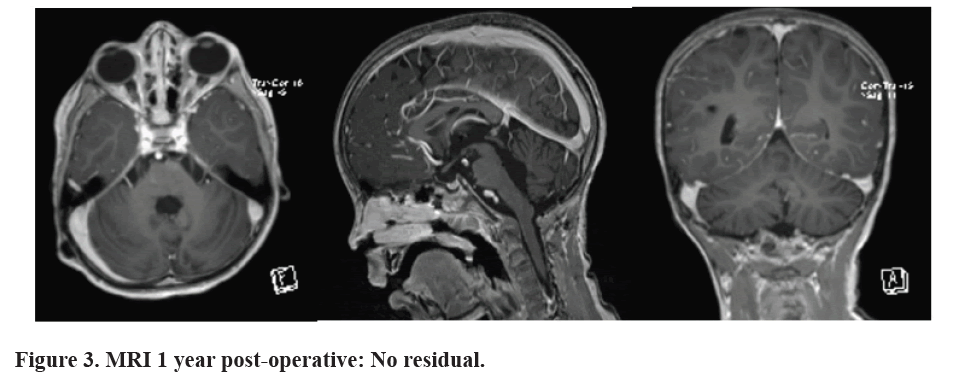
as well. His medications were finally stopped
almost a year later after gradual tapering down as
the patient continued to improve to the point of
complete recovery.
Discussion
Posterior fossa mutism syndrome is a rare complication of brain tumor excision surgery. Few case reports and case studies on this subject have been published. An even fewer number of studies have been published on the use of lorazepam as a treatment modality for it. Risk factors to developing this syndrome were identified to include pediatric age group, midline tumor and midline incision [6].
We present a patient who was unfortunate to developed posterior fossa syndrome. He is a toddler boy who was diagnosed and treated for ependymoma. He was later presented with a postoperative complication which was identified to be posterior fossa mutism syndrome.
The precise pathophysiology of posterior fossa mutism syndrome is not yet fully understood. There are multiple proposed theories for the pathophysiology of this syndrome and it is believed that the pathogenesis is most likely to be multifactorial.
Its pathophysiology is believed to result from the injury of the Dentato-Thalamo-Cortical (DTC) pathway, leading to Cerebro-Cerebellar Diaschisis (CCD) [7].
Like this presented case, most cases that were displayed in the literature were from a pediatric age group. It was also mentioned earlier in this paper that most patients that end up with the complication of posterior fossa mutism can have spontaneous recovery. However, studies show that recovery is usually partial and incomplete [8]. Studies show that even though mutism is transient, most patients are usually left with dysarthria [9]. This was not the case with the patient shown in our case. He showed subtle progressive improvement shortly after the operation and ended in full resolution of his mutism without the commonly occurring dysarthria.
The management is usually supportive but can include speech and occupational therapy. Most patients with posterior fossa mutism are expected to have spontaneous and complete recovery of most symptoms. However, most patients can be left with slowed speech and ataxic dysarthria [10]. This was definitely not the case with our patient who was treated with lorazepam and showed full recovery of his mutism. His speech was back to normal and matches speech of children his age.
Few pharmacological treatments had been studied including Bromocriptine, fluoxetine, haloperidol, risperidone, delorazepam, and zolpidem have been tested as potential treatments for a certain condition. However, the studies conducted on these drugs involved small sample sizes, making it difficult to draw any meaningful conclusions. The beneficial effects of these drugs usually appear at least 24 hours after the first administration, and complete recovery can take several months, which further complicates the assessment of their contribution to healing.
On the other hand, a study reported that midazolam was able to resolve post-operative Centers for Medicare and Medicaid Services (CMS) within a few minutes after intravenous administration in a 17-year-old boy who had undergone a fourth- ventricle choroid plexus papilloma resection [11].
The mechanism of action of Lorazepam and other benzodiazepine medications like Midazolam work by increasing ionotropic Gamma-Aminobutyric Acid (GABA)-ergic stimulation, an inhibitor of neural activity. An inhibitory effect of this drug on the direct and indirect basal ganglia pathways that regulate the excitatory output of the thalamus. The final result is a reduction of inhibition of the thalamus via the striatum, an outcome similar to what is obtained with bromocriptine administration [12].
The management of patients with posterior fossa syndrome is multi-disciplinary team is indeed needed for such patients. In this case we present, the patient was managed by a multi-disciplinary team that included a neurologist, neurosurgeon, oncologist, psychiatrist and a physiotherapist (Figures 1-3).
Conclusion
Posterior fossa mutism syndrome is a
complication of posterior fossa surgery. It is
usually transient but the exact duration to witch
symptoms improve differs from one patient to
another. The exact pathophysiology for how it
develops is still not fully understood. A multidisciplinary
team is needed for the management
of such patients. This includes, neurosurgeons,
neurologists, oncologists, psychiatrist and speech
and occupational therapists. No pharmacological
management protocol has been established for
Posterior fossa mutism yet. Lorazepam shows
promising results. However, further studies are
definitely needed to confirm its effects.
Posterior fossa mutism represents a complex and
challenging phenomenon observed predominantly
in pediatric patients following surgical
interventions in the posterior fossa region. While
its exact mechanisms remain elusive, current
research suggests multifactorial involvement,
including disruption of cerebellar pathways, direct surgical trauma, and neuroinflammatory
responses.
References
- Catsman-Berrevoets CE, Aarsen FK. The spectrum of neurobehavioural deficits in the posterior fossa syndrome in children after cerebellar tumour surgery. Cortex. 2010;46(7):933-946.
[Crossref][Google Scholar][PubMed]
- Kirk EA, Howard VC, Scott CA. Description of posterior fossa syndrome in children after posterior fossa brain tumor surgery. J Pediatr Oncol Nurs. 1995;12(4):181-187.
[Crossref][Google Scholar][PubMed]
- Gadgil N, Hansen D, Barry J, Chang R, Lam S. Posterior fossa syndrome in children following tumor resection: Knowledge update. Surg Neurol Int. 2016;7(Suppl 6):S179-S183.
[Crossref][Google Scholar][PubMed]
- Khan RB, Patay Z, Klimo Jr P, Huang J, Kumar R, et al. Clinical features, neurologic recovery, and risk factors of postoperative posterior fossa syndrome and delayed recovery: A prospective study. Neuro Oncol. 2021;23(9):1586-1596.
[Crossref][Google Scholar][PubMed]
- Lanier JC, Abrams AN. Posterior fossa syndrome: Review of the behavioral and emotional aspects in pediatric cancer patients. Cancer. 2017;123(4):551-559.
[Crossref][Google Scholar][PubMed]
- Pollack IF. Posterior fossa syndrome. Int Rev Neurobiol. 1997;41:411-432.
[Crossref][Google Scholar][PubMed]
- Ashida R, Nazar N, Edwards R, Teo M. Cerebellar mutism syndrome: An overview of the pathophysiology in relation to the cerebrocerebellar anatomy, risk factors, potential treatments, and outcomes. World Neurosurg. 2021;153:63-74.
[Crossref][Google Scholar][PubMed]
- Wibroe M, Cappelen J, Castor C, Clausen N, Grillner P, et al. Cerebellar mutism syndrome in children with brain tumours of the posterior fossa. BMC cancer. 2017;17(1):1-7.
[Crossref][Google Scholar][PubMed]
- Küper M, Timmann D. Cerebellar mutism. Brain Lang. 2013;127(3):327-333.
[Crossref][Google Scholar][PubMed]
- Gündüz HB, Yassa MI, Ofluoğlu AE, Postalci L, Erhan EM. Cerebellar mutism syndrome after posterior fossa surgery: A report of two cases of pilocytic astrocytoma. Noro Psikiyatr Ars. 2013;50(4):368-371.
[Crossref][Google Scholar][PubMed]
- Fabozzi F, Margoni S, Andreozzi B, Musci MS, Del Baldo G, et al. Cerebellar mutism syndrome: From pathophysiology to rehabilitation. Front Cell Dev Biol. 2022;10:1082947.
[Crossref][Google Scholar][PubMed]
- Nicita F, Paiano M, Liberatore M, Spalice A, Papoff P, et al. Sudden benzodiazepine-induced resolution of post-operative pediatric cerebellar mutism syndrome: A clinical-SPECT study. Acta Neurochir (Wien). 2017;159:475-479.
[Crossref][Google Scholar][PubMed]
Citation: Lorazepam for the Management of Posterior Fossa Mutism: A Case Report ASEAN Journal of Psychiatry, Vol. 25 (5) May, 2024; 1-5.