Introduction
Intensive Care Units (ICUs) represent some of the most demanding environments in healthcare, requiring constant vigilance, rapid decision-making, and the management of life-threatening situations. Healthcare professionals working in ICUs, particularly nurses and healthcare assistants, are frequently exposed to important levels of
stress due to the need to care for critically ill
patients, execute complex medical interventions
and respond to unpredictable emergencies
[1]. Over time, this chronic exposure to such
high-stress conditions can lead to burnout a
syndrome characterized by emotional exhaustion,
depersonalization, and a diminished sense of
personal accomplishment [2].
Burnout has been extensively studied across
various healthcare settings due to its significant
implications. Research shows that burnout
adversely affects the mental and physical wellbeing
of healthcare providers and compromises
the quality of patient care. In ICU settings, where
patient outcomes are linked to the performance
and mental state of the healthcare team, the
consequences of burnout can be particularly
severe [3]. Studies have highlighted correlations
between burnout and negative outcomes such as
increased absenteeism, reduced job satisfaction
and higher turnover rates, all of which can impair
clinical judgment and patient safety [4]. Despite
the substantial body of literature on burnout
in healthcare, there remains a significant gap
in understanding how objective physiological
indicators of stress, such as heart rate variability
(HRV), relate to psychometric assessments of
stress among ICU personnel [5].
HRV is increasingly recognized as a reliable and
non-invasive biomarker of Autonomic Nervous
System (ANS) function, reflecting the balance
between the Sympathetic Nervous System (SNS)
and the Parasympathetic Nervous System (PNS)
[6]. The SNS is responsible for the body’s “fight
or flight” response, while the PNS governs “rest
and digest” activities. HRV measures the variation
in time intervals between heartbeats, providing
insights into autonomic regulation and overall
physiological stress levels. A higher HRV typically
indicates a healthy balance between the SNS
and PNS, suggesting good autonomic flexibility
and resilience to stress. Conversely, a lower
HRV is associated with increased sympathetic
activity, reduced parasympathetic activity and
consequently, higher levels of physiological
stress. While HRV has been validated as a stress
indicator in various populations, including
athletes, military personnel and general healthcare
workers, research specifically focusing on HRV in
ICU personnel is limited [7]. Studies in other highstress
professions, such as law enforcement and
emergency medical services, have demonstrated that HRV can effectively monitor stress and predict
burnout, suggesting its potential applicability in
ICU settings [8].
In addition to HRV, psychometric tools provide
valuable insights into the subjective experience
of stress. The State-Trait Anxiety Inventory
(STAI) is widely used to assess both state and trait
anxiety, offering a comprehensive evaluation of
an individual’s anxiety levels [9]. The Perceived
Stress Scale (PSS-14) measures the extent to which
participants perceive their lives as unpredictable,
uncontrollable and overloaded, providing a general
assessment of perceived stress [10]. The Nursing
Stress Scale (NSS) is specifically designed to
evaluate stress related to various aspects of the
nursing profession, including workload, patient
care and interpersonal relationships. These
tools have been validated in healthcare settings,
including among Spanish- speaking populations,
making them appropriate for use in this study
[11]. Previous research has shown that higher
perceived stress levels, as measured by the PSS-
14, are associated with lower HRV, indicating
greater physiological stress. However, few studies
have integrated these approaches in ICU settings,
where stress levels are exceptionally high. This
study aims to bridge this gap by combining
HRV analysis with psychometric assessments to
provide a comprehensive evaluation of stress in
ICU nursing staff.
Shift work is another well-documented stressor in
healthcare, particularly in ICUs where patient care
is required around the clock. Nurses and healthcare
assistants working night shifts or extended hours
often report higher levels of stress and burnout
compared to those on regular day shifts [12]. The
disruption of circadian rhythms, lack of adequate
rest and social isolation associated with night
shifts contribute to this increased stress burden.
Additionally, extended shifts can lead to fatigue,
impairing cognitive function and decision-making
abilities, which are critical in ICU settings. Studies
have shown that night shift work is associated
with lower HRV, indicating higher physiological
stress and an increased risk of burnout. Despite
these findings, the specific impact of shift type
and length on both HRV and psychometric stress
measures in ICU settings has not been thoroughly
explored.
Given the high prevalence of stress and burnout
among ICU staff and the growing interest in
HRV as a biomarker for stress, this study seeks to explore the utility of HRV in conjunction with
psychometric assessments. By examining the
correlations between HRV metrics and subjective
stress measures across different shifts, this study
aims to identify specific patterns and predictors
of stress and burnout in this high-risk population.
Additionally, the study will explore the influence
of demographic and lifestyle factors on these stress
responses, contributing to the broader literature on
occupational stress and burnout in healthcare.
Materials and Methods
Study design
This observational cross-sectional pilot study
was conducted to explore the relationship
between Heart Rate Variability (HRV) metrics
and psychometric assessments of stress in ICU
nursing staff. The study took place over a threemonth
period at a University Hospital in Madrid,
Spain (from 5 February, 2024 to 26 April, 2024).
Given the exploratory nature of this study and the
small sample size, the primary goal was to identify
potential correlations and trends that could inform
future, larger-scale research. Due to the study’s
cross-sectional design, the findings should be
interpreted with caution, as no causal inferences
can be made and generalizability is limited. Future
research could benefit from longitudinal designs
and larger samples, potentially expanding the
scope to other high-stress hospital settings, such
as emergency rooms and operating theaters.
Participants
The original sample consisted of 26 ICU healthcare
professionals; however, two participants were
excluded from the analysis due to errors in signal
acquisition and processing, resulting in a final
sample size of twenty-four participants. This
sample size was deemed appropriate for a pilot
study aimed at identifying preliminary trends and
correlations. Participants were recruited based
on convenience sampling, with 54% of the ICU
personnel volunteering to participate. The final
sample included 62.5% registered nurses and
37.5% healthcare assistants (TCAEs)
Inclusion criteria
• Full-time employment in the ICU with at least
one year of experience.
• Age between 25 and 50 years to minimize
age-related variability in HRV, aligning with the actual demographic distribution of the
ICU staff.
• No history of cardiovascular disease or use of
medications that could influence HRV (e.g.,
beta-blockers, antiarrhythmic).
• Willingness to participate, with all participants
providing informed consent. The study was
conducted in accordance with the principles
outlined in the declaration of Helsinki,
ensuring strict adherence to ethical guidelines
for medical research involving human
subjects.
Exclusion criteria
• Presence of any medical condition that could
interfere with HRV readings or psychometric
assessments.
• Recent surgery or trauma that could affect
autonomic nervous system function.
• Errors in signal acquisition and processing
with the Biosignalplux device, leading to the
exclusion of two participants from the final
analysis.
Participants were balanced in terms of gender
and shift type (day vs night) to ensure that the
sample was representative of the broader ICU
staff population. Demographic data, including
age, gender, years of experience and typical shift
patterns, were collected through a structured
questionnaire. A comprehensive lifestyle and
health questionnaire was also administered to
gather information on participants’ general health
status, lifestyle habits and any factors that could
influence stress levels or HRV.
Psychometric assessments
To evaluate the subjective experience of stress
and anxiety among participants, several validated
psychometric instruments were employed:
State-Trait Anxiety Inventory (STAI): Measures
both the current level of anxiety (state anxiety) and
the general tendency to experience anxiety (trait
anxiety), consisting of two subscales with twenty
items each, scored on a four-point Likert scale.
Perceived Stress Scale (PSS-14): Assesses the
extent to which participants perceive their lives
as unpredictable, uncontrollable and overloaded,
with fourteen items scored from 0 (never) to 4 (very often).
Nursing Stress Scale (NSS): Specifically designed for nursing staff, this scale measures stress related to various aspects of the nursing profession, including workload, patient care and interpersonal relationships, with thirty-four items scored on a five-point Likert scale.
Visual Analogue Scale for Stress (VASS): Administered at the beginning and end of the shift, allowing participants to rate their perceived stress on a continuum from 0 (no stress) to 100 (maximum stress).
These tools have been previously validated in Spanish-speaking populations, including healthcare settings, and were deemed appropriate for this study. Although there is an inherent risk of social desirability bias in self-reporting tools, participants were encouraged to provide honest responses to ensure the reliability of the data. The original Spanish versions of the STAI, PSS-14, and NSS questionnaires used in this study are provided as supplementary material to this paper (S1-Original Questionnaires).
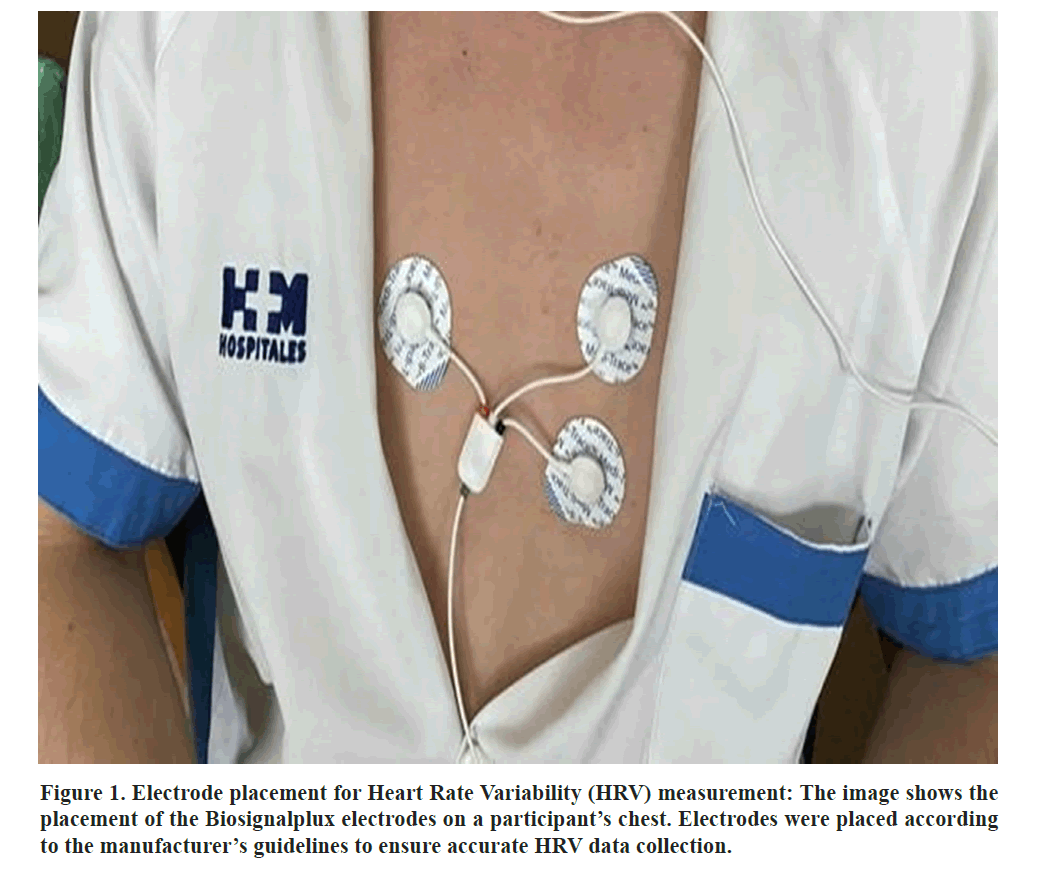
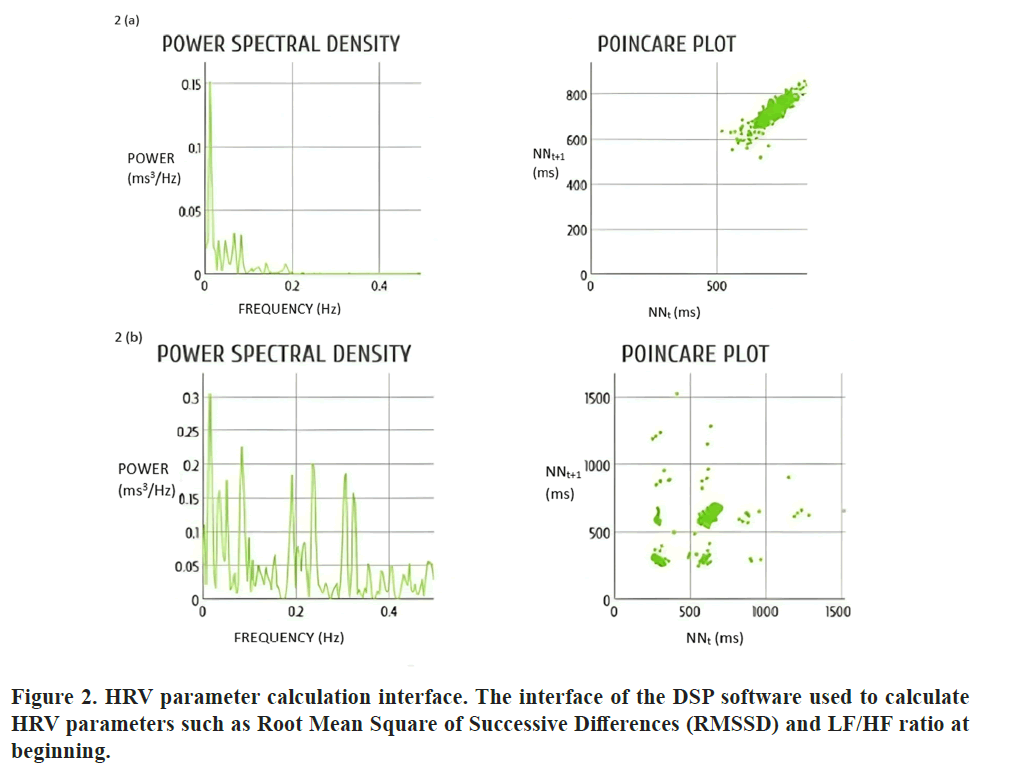
Biometric measurements
HRV was the primary biometric indicator used to assess stress levels in this study. HRV data were collected using the Biosignalplux system, a portable ECG monitoring device that records real time heart rate data and allows for detailed HRV analysis. The device was attached to participants using chest electrodes at the start and end of their shifts, with HRV measurements taken while participants were seated and at rest for 10 minutes before the start of the shift and another 10 minutes after the end of the shift. This standardized procedure ensured that the HRV data were collected in a controlled environment, minimizing potential confounding factors such as physical activity or movement (Figures 1 and 2).
Key HRV parameters analyzed
Root Mean Square of Successive Differences (RMSSD): A time-domain measure of HRV that reflects short term variations in heart rate and is closely related to parasympathetic activity.
Percentage of Consecutive NN Intervals That Differ by More Than 50 ms (pNN50): Indicates the proportion of differences between adjacent heartbeats that exceed fifty milliseconds, associated with parasympathetic regulation.
Low-Frequency to High-Frequency Ratio (LF/HF Ratio): Represents the balance between sympathetic and parasympathetic nervous activity, with a higher ratio indicating increased sympathetic activity and reduced parasympathetic activity, often associated with stress.
Secondary biometric measures
Blood pressure: Measured at the beginning, mid-point and end of each shift to monitor potential cardiovascular responses to stress.
Respiratory rate and oxygen saturation: Monitored continuously alongside HRV to provide a comprehensive overview of physiological responses.
Electrode placement followed the manufacturer’s instructions, and participants were in a resting state during measurements to minimize potential movement artifacts. Secondary biometric measures were taken simultaneously with HRV data collection to ensure consistency.
Procedure
Prior to data collection, participants received a detailed explanation of the study’s objectives and procedures. Informed consent was obtained and participants were assured of the confidentiality of their data. Psychometric assessments and demographic questionnaires were completed at home before the beginning of the recording phase. Each participant was equipped with the Biosignalplux system at the beginning of their shift. The device was calibrated to ensure accurate data collection and participants were instructed to continue their regular duties without altering their routines.
The study was designed to include both day and night shifts, with participants monitored during a minimum of two shifts. This approach allowed for a comparison of HRV and stress levels across different working conditions. HRV data were transmitted to a secure server for analysis immediately after each shift. Psychometric data were entered into a database, with each participant assigned a unique identifier to maintain anonymity. Data were anonymized and stored securely, with access limited to the principal investigator.
Data analysis
Statistical analysis was conducted using SPSS version 25.0. The primary analysis involved comparing HRV metrics across different shift types (day vs night) and correlating these metrics with psychometric scores and demographic data. After the results were obtained and classified, a sequential statistical analysis was conducted. Initially, the normality of the samples was assessed using both the Kolmogorov-Smirnov and Shapiro-Wilk tests, considering the small sample size. Since several parameters did not follow a normal distribution and the sample size was limited, it was decided to use non-parametric tests for the analysis.
Statistical methods
Wilcoxon signed-rank tests: Used for comparative analysis of HRV and psychometric data at the start and end of shifts.
Spearman correlations: Employed to assess relationships between HRV metrics and psychometric scores.
Mann-Whitney U tests: Applied for comparative analysis between day and night shifts.
Multiple Regression Analysis (MANOVA): Conducted to explore interactions between demographic/medical variables and biometric/psychometric stress indicators, acknowledging that multi collinearity could pose challenges given the small sample size.
Significance was set at p<0.05 for all analyses. Results were interpreted in the context of existing literature on HRV and occupational stress in healthcare professionals, with particular attention to the implications for managing stress in ICU settings. The pilot nature of the study and the small sample size necessitate caution in generalizing the findings, but they provide a basis for future research and potential interventions in similar high-stress environments.
Results
Demographic characteristics
The study included twenty-four participants, of whom 62.5% were registered nurses, and 37.5% were healthcare assistants (TCAEs). The mean age of participants was 38 years, with 70.83% being female. Most participants (50%) worked 12-hour shifts, and 54.17% were assigned to the morning shift. On average, participants had 3.8 years of experience in their current roles. The average household income was reported as €3,000, with nearly half of the participants indicating caregiving responsibilities for dependents (Table 1).
Table 1. Demographic characteristics.
| Characteristic |
Percentage (%) |
| Gender |
| Female |
70.83 |
| Male |
29.17 |
| Age |
| <30 years |
25 |
| 30-40 years |
45.83 |
| 40-50 years |
12.5 |
| >50 years |
16.67 |
| Household income |
| < € 2500 |
33.34 |
| € 2500-4500 |
54.16 |
| > € 4500 |
12.5 |
| Job position |
| Registered Nurse (DUE) |
62.5 |
| Healthcare Assistant (TCAE) |
37.5 |
| Years of service |
| <5 years |
66.67 |
| >5 years |
33.33 |
| Shift |
| Morning |
54.17 |
| Afternoon |
12.5 |
| Night |
33.33 |
| Shift duration |
| 7 hours |
29.17 |
| 10 hours-12 hours |
70.83 |
Lifestyle habits were self-reported, with most participants consuming alcohol occasionally. Tobacco use was reported by 30% of participants, though less than 10% were significant smokers. Additionally, 85% consumed 1-3 cups of coffee daily, and 90% engaged in regular physical activity. Notably, over half of the participants felt that stress negatively impacted their work performance, with 62.5% having considered leaving the profession and nearly 30% reporting having experienced suicidal ideation at some point (Tables 2 and 3).
Table 2. Lifestyle and consumption habits.
| Characteristic |
Percentage (%) |
| Alcohol consumption |
| Never |
12.5 |
| Occasionally |
87.5 |
| Tobacco consumption |
| Never |
70.83 |
| Regular (More than three cigarettes/day) |
16.66 |
| Coffee consumption |
| None |
12.5 |
| 1-3 cups/day |
83.33 |
| Recreational drug use |
| Never |
87.5 |
| Occasionally |
12.5 |
| Physical activity |
| None |
12.5 |
| Regular |
50 |
| Perceived stress impact on work |
| Yes |
54.16 |
| Considered leaving profession |
| Yes |
62.5 |
| Considered self-harm |
| Yes |
29.16 |
Table 3. Health status and medication use.
| Condition |
Yes (%) |
| Cardiovascular disease |
4.17 |
| Hypertension |
4.17 |
| Dyslipidemia |
4.17 |
| Depression |
8.33 |
| Anxiety |
50 |
| Thyroid hormone use |
8.33 |
| Antidepressant use |
16.67 |
| Anxiolytic use |
8.33 |
Statistical analysis and normality testing
Given the small sample size and the non-normal distribution of some parameters, non-parametric tests were applied throughout the analysis.
This approach was deemed appropriate for identifying potential correlations in this pilot study, with the aim of informing larger-scale research.
Basic physiological variables
Shift duration impact: The Wilcoxon signed-rank test revealed that only the perceived stress scale exhibited a statistically significant change (p<0.05), increasing from the beginning to the end of the shift. This finding aligns with expectations that stress levels would escalate during the shift, consistent with previous research.
Shift type comparison: The Kruskal-Wallis test showed no significant differences in most physiological variables (e.g., heart rate, oxygen saturation, systolic blood pressure) across different shifts (morning, afternoon, night). However, diastolic blood pressure demonstrated a significant variation (p=0.028), suggesting that different shift types might exert varying levels of cardiovascular stress.
Work shift duration: Comparisons between normal and extended shifts using the Kruskal-Wallis test revealed no statistically significant differences in the measured physiological variables, except for diastolic blood pressure, which is a well-documented indicator of stress levels in the literature.
Biometric variables
Shift duration impact: Wilcoxon signed-rank tests indicated no significant differences in HRV metrics (RMSSD, pNN50, LF/HF ratio) between the beginning and end of shifts. This stability in HRV suggests that the physiological impact of stress, as measured by HRV, remained consistent throughout the work shift. However, this finding may be influenced by the small sample size, limiting the detection of subtler variations.
Shift type comparison: The Kruskal-Wallis test revealed that most HRV parameters did not significantly differ between morning, afternoon and night shifts. However, the LF/HF ratio at the beginning of the shift presented a significant difference across shifts (p=0.043), indicating variations in autonomic nervous system activity depending on shift timing. This finding is consistent with the literature, which associates night shifts with increased sympathetic nervous system activity and higher stress levels.
Work shift duration: Like the physiological variables, no significant differences were found in HRV metrics between normal and extended shifts, except for the LF/HF ratio, which showed a significant difference (p=0.033). This suggests that longer shifts might contribute to an imbalance in autonomic regulation, particularly in the sympathetic-parasympathetic balance, which could be indicative of elevated stress levels.
Psychometric variables
The psychometric scales used in the study demonstrated high reliability, with a Cronbach’s alpha of 0.883 for the STAI scale (Table 4).
Table 4. Summary of psychometric scale results.
| ID |
State anxiety score |
Trait anxiety score |
PSS score |
NSS score |
| 1 |
25 |
21 |
37 |
45 |
| 2 |
12 |
21 |
25 |
35 |
| 3 |
25 |
27 |
28 |
22 |
| 4 |
18 |
14 |
20 |
25 |
| 5 |
16 |
11 |
19 |
33 |
| 6 |
32 |
29 |
23 |
38 |
| 7 |
27 |
32 |
33 |
35 |
| 8 |
13 |
26 |
20 |
46 |
| 9 |
16 |
14 |
17 |
41 |
| 10 |
18 |
16 |
22 |
37 |
| 11 |
10 |
4 |
11 |
41 |
| 12 |
15 |
10 |
20 |
28 |
| 13 |
27 |
31 |
29 |
45 |
| 14 |
12 |
10 |
19 |
20 |
| 15 |
11 |
8 |
21 |
36 |
| 16 |
15 |
16 |
22 |
24 |
| 17 |
20 |
26 |
28 |
34 |
| 18 |
48 |
42 |
44 |
28 |
| 19 |
13 |
16 |
18 |
24 |
| 20 |
16 |
21 |
30 |
53 |
| 21 |
28 |
25 |
31 |
79 |
| 22 |
17 |
10 |
30 |
40 |
| 23 |
12 |
17 |
18 |
32 |
| 24 |
20 |
33 |
44 |
48 |
Psychometric scales and their respective score ranges: STAI-State (range 20-80), STAI-Trait (range 20-80), PSS (range 0-40) and NSS (higher scores indicate greater levels of job-related stress).
The following correlations were observed:
VASS and axiety: Initial VASS scores were moderately correlated with state anxiety (STAI A_E) (r=0.407, p<0.05) and strong correlations were found between state anxiety (STAI A_E) and both trait anxiety (STAI A_R) (r=0.793, p<0.001) and Perceived Stress (PSS) (r=0.703, p<0.001). These correlations highlight the interrelationship between anxiety and perceived stress among ICU staff, which is consistent with findings from other studies in similar populations
Shift comparisons: Multiple comparisons using the Kruskal-Wallis test, adjusted by Turkey’s HSD and Bonferroni corrections where applicable, indicated no significant differences in psychometric variables across different shifts or between normal and extended shifts. This lack of significant differences is due to the small sample size, which may have limited the statistical power to detect differences.
Correlations between demographic variables and psychometric tests
Income and anxiety: Higher income levels were significantly correlated with lower levels of state anxiety (STAI_A_E: r=-0.443, p=0.030) and trait anxiety (STAI_A_R: r=-0.489, p=0.015). This finding suggests that a better economic status may mitigate anxiety levels among ICU staff.
Lifestyle factors
Physical activity: There was a positive correlation between initial VASS scores and participation in sports (r=0.422, p=0.040), suggesting that individuals with higher initial stress may engage more in physical activities, potentially as a coping strategy.
Health status
Medication use: The use of antidepressants was highly correlated with the use of anxiolytics (r=0.674, p<0.001), indicating that these medications are often co-prescribed for managing mental health conditions in this population.
Self-perceived stress
Anxiety and stress: Both state and trait anxiety were significantly correlated with Perceived Stress (PSS) and the initial VASS score. High levels of anxiety were also associated with lower well-being (STAI_A_E: r=-0.599, p=0.002; STAI_A_R: r=-0.459, p=0.024) and increased thoughts of “giving up” or “abandoning” (STAI_A_R: r=0.723, p<0.001). These findings highlight the significant impact of anxiety and stress on mental health, suggesting a potential area for targeted interventions.
Global correlations between biometric and psychometric variables
When analyzing the data globally across all time points (both start and end of shifts), a consistent pattern emerged where higher levels of psychological stress, as measured by validated psychometric scales, were associated with lower HRV metrics. This pattern supports HRV as a reliable indicator of autonomic dysregulation in response to stress. The high inter correlation among HRV measures further reinforces their validity as robust indicators of cardiac autonomic function, consistent with findings in other studies of occupational stress in healthcare settings.
Discussion
This study explored the relationships between biometric stress variables, derived from Heart Rate Variability (HRV) analysis and psychometric stress variables among ICU nursing staff. Additionally, the study examined the impact of shift type and duration on these variables and investigated the influence of demographic factors, health status and lifestyle habits on stress and anxiety. The findings contribute to a growing body of literature on occupational stress in healthcare, with specific implications for ICU settings.
HRV and psychometric stress measures
A significant negative correlation was observed between HRV metrics, particularly the LF/HF ratio and perceived stress levels, as measured by the Visual Analogue Scale for Stress (VASS). This finding aligns with previous research, such as the study by Xinxia Li et al., which demonstrated a significant association between HRV and perceived stress levels among nurses [13]. The negative correlation suggests that higher perceived stress is associated with lower HRV, indicating increased physiological stress. These results support the use of HRV as a potential objective marker for stress in ICU nursing staff, providing a physiological correlation to subjective experiences of stress.
However, it is important to note that the stability of HRV metrics across shifts, with no significant changes observed between the beginning and end of shifts, might be influenced by the small sample size. This stability could suggest a level of physiological resilience among the participants, or it might reflect the limitations of detecting subtler variations in autonomic regulation with the available sample [14]. The lack of significant differences in HRV metrics between different shifts (morning, afternoon, night) further complicates the interpretation, although the significant variation in the LF/HF ratio across shifts points to potential differences in autonomic nervous system activity that warrant further investigation.
Impact of shift work on stress
The study found that shift type and duration significantly influenced certain stress indicators. Night shifts were associated with a higher LF/HF ratio at the beginning of the shift, indicating greater sympathetic nervous system activity and higher stress levels. This finding is consistent with existing literature that links night shifts to increased physiological stress and reduced HRV [15]. For example, Varghese et al., found that night shift work was associated with lower HRV among healthcare workers, which is indicative of elevated stress [16].
Extended shifts also exacerbated stress, as evidenced by the significant difference in diastolic blood pressure between normal and extended shifts [17]. While HRV metrics did not show significant changes based on shift duration, the observed variations in blood pressure suggest that extended shifts may still pose a cardiovascular strain on ICU staff. This finding underscores the need for further research into the physiological impacts of extended work hours, especially in high-stress environments like ICUs.
Psychometric assessments and their correlations
Psychometric assessments revealed strong correlations between state and trait anxiety, perceived stress and the initial VASS scores. These correlations indicate that individuals with higher baseline anxiety levels are more likely to report elevated stress throughout their shifts. This finding is consistent with studies such as those by Lesage et al., which demonstrated a significant association between anxiety symptoms and psychological stress among health workers [18]. The persistence of anxiety and stress levels throughout the work shift suggests that these factors are deeply intertwined and may contribute to the overall burden of stress experienced by ICU staff.
Demographic and lifestyle influences on stress
Higher income levels were found to correlate significantly with lower levels of state and trait anxiety, suggesting that financial stability may serve as a buffer against stress and anxiety in this population. This is in line with the broader literature on socioeconomic status and mental health, where higher income often correlates with better coping mechanisms and lower perceived stress [19].
Additionally, physical activity was positively correlated with initial stress levels, indicating that those who engage in regular exercise might be using it as a coping strategy to manage higher baseline stress. This aligns with existing research suggesting that physical activity can serve as a protective factor against stress and burnout [20]. The significant correlation between the use of antidepressants and anxiolytics further highlights the mental health challenges faced by ICU staff and suggests that medication use may be common among those experiencing elevated levels of stress and anxiety [21].
Implications for practice
The findings of this study have several practical implications for managing stress and preventing burnout among ICU staff. The significant correlations between HRV and psychometric measures of stress suggest that HRV monitoring could be integrated into routine occupational health assessments to provide early warnings of stress-related health risks. By identifying shifts associated with increased stress, such as night shifts and extended work hours, healthcare administrators can implement targeted interventions, such as rotating shifts, reducing shift duration and promoting physical activity as a coping strategy.
Furthermore, the strong association between anxiety, stress, and income levels suggests that financial incentives or support might play a role in reducing stress. Programs aimed at improving the financial well-being of healthcare workers, alongside traditional stress management and mental health support services, could be beneficial.
Limitations and Future Scope
This study has some limitations that should be addressed in future research. The small sample size is the most significant limitation, as it restricts the generalizability of the findings and may have prevented the detection of subtler differences in HRV metrics. The cross-sectional design also limits the ability to draw causal inferences between HRV, psychometric measures, and shift work. Future studies should include larger, more diverse samples and consider longitudinal designs to capture the progression of stress and burnout over time. Expanding the scope to include other high-stress hospital settings, such as emergency rooms and operating theaters, would also provide valuable comparative data.
Additionally, the study’s reliance on self-reported data for psychometric assessments introduces the possibility of social desirability bias, where participants might underreport their stress levels. To reducing this, future research could incorporate more objective measures of stress, such as cortisol levels, alongside HRV and psychometric assessments.
Conclusion
This pilot study highlights the potential of HRV as an objective measure of stress in ICU nursing staff, with significant correlations observed between HRV metrics and psychometric assessments. The findings suggest that HRV could be a valuable tool for monitoring stress in real- time and identifying individuals at risk of burnout. However, further research with larger samples and a longitudinal approach is needed to validate these results and explore their implications for occupational health practices in ICU settings. The integration of HRV monitoring with traditional stress management programs could lead to more effective interventions, improving the well-being and performance of ICU staff.
However, this study also highlights the need for further research to refine these integrated approaches and validate their effectiveness in larger, more diverse populations. Future studies should explore longitudinal designs to assess the impact of interventions over time and consider additional variables that may influence stress and burnout in ICU settings.
Acknowledgements
We sincerely thank all the nurses and healthcare assistants (TCAEs) who participated in this study. Your contributions were invaluable, and this research would not have been possible without your involvement. We appreciate your time and effort in helping us better to understand the stress and burnout experienced in ICU setting.
Declarations
Ethical committee consent
This study received ethical approval from the HM Hospitals Research Ethics Committee (Code: 18.12.1339.GHM) and involved twenty-six consenting ICU health personnel. All participants provided written informed consent, and their data were anonymized to protect confidentiality.
Availability of data and materials
The datasets used and/or analyzed during the current study.
Authors’ contributions
Alberto Rubio-Lopez designed the study, collected the data, performed the statistical analysis, and wrote the study as the principal investigator. Teresa Sierra-Puerta participated in the performance tests and in the design and collection of biometric parameters, collected the data and participated writing of the paper. Alejandro Rubio Navas participated in the performance tests and in the design and collection of biometric parameters.
References
- Original A, Longhi A, Alberto Bezerra Tomaz C. HRV and emotions in intensivists original article. Rev Bras Cardiol. 2010.
- Andrade-Méndez B, Arias-Torres DO, Gómez-Tovar LO. Alarm fatigue in the intensive care unit: Relevance and response time. Intensive Nursing. 2020;31(3):147-153.
[Crossref][Google Scholar][PubMed]
- Arrogante O, Aparicio-Zaldivar EG. Burnout syndrome in intensive care professionals: Relationships with health status and wellbeing. Intensive Nursing. 2020;31(2):60-70.
[Crossref][Google Scholar][PubMed]
- Shah SG, Ahmed A, Ahmed A, Ikram K, Mirza A, et al. Assessment of occupational based stress and internal coherence related with quality of life through Heartrate Variability (HRV)-a cross sectional study. J Health Rehabil Res. 2024;4(2):1591-1596.
[Crossref][Google Scholar]
- Järvelin-Pasanen S, Sinikallio S, Tarvainen MP. Heart rate variability and occupational stress-systematic review. IndHealth. 2018;56(6):500-511.
[Crossref][Google Scholar][PubMed]
- Ueno S, Huang R, Fujita S. Quantitative stress analysis using heart rate variability. IIAE. 2019;41-46.
[Crossref][Google Scholar]
- Rieger A, Stoll R, Kreuzfeld S, Behrens K, Weippert M. Heart rate and heart rate variability as indirect markers of surgeons’ intraoperative stress. Int Arch Occup Environ Health. 2014;87:165-174.
[Crossref][Google Scholar][PubMed]
- Thielmann B, Pohl R, Böckelmann I. Heart rate variability as a strain indicator for psychological stress for emergency physicians during work and alert intervention: A systematic review. J Occup Med Toxicol. 2021;16(1):24.
[Crossref][Google Scholar][PubMed]
- Knowles KA, Olatunji BO. Specificity of trait anxiety in anxiety and depression: Meta-analysis of the state-trait anxiety inventory. Clin Psychol Rev. 2020;82:101928.
[Crossref][Google Scholar][PubMed]
- Teresi JA, Ocepek-Welikson K, Ramirez M, Kleinman M, Ornstein K, et al. Evaluation of the measurement properties of the Perceived Stress Scale (PSS) in Hispanic caregivers to patients with Alzheimer’s disease and related disorders. Int Psych. 2020;32(9):1073-1084.
[Crossref][Google Scholar][PubMed]
- Porcel-Gálvez AM, Barrientos-Trigo S, Bermúdez-García S, Fernández-García E, Bueno-Ferrán M, et al. The nursing stress scale-spanish version: An update to its psychometric properties and validation of a short-form version in acute care hospital settings. Int J Environ Res Public Health. 2020;17(22):8456.
[Crossref][Google Scholar][PubMed]
- Tomaszewska K, Kowalczuk K, Majchrowicz B. Relationships between job satisfaction, occupational burnout and rationing of care among intensive care unit nurses. Front Public Health. 2024;12:1400169.
[Crossref][Google Scholar][PubMed]
- Li X, Zhu W, Sui X, Zhang A, Chi L, et al. Assessing workplace stress among nurses using heart rate variability analysis with wearable ECG device-a pilot study. Front Public Health. 2022;9:810577.
[Crossref][Google Scholar][PubMed]
- Luo J, Zhang G, Su Y, Lu Y, Pang Y, et al. Quantitative analysis of heart rate variability parameter and mental stress index. Front Cardiovasc Med. 2022;9:930745.
[Crossref][Google Scholar][PubMed]
- Johnson K, Braksick S, St. Louis E, Somers V, Olson E, et al. 0291 Attending Physician Perceptions of Nightshift Work in the ICU: Results from a Large Tertiary Medical Center. Sleep. 2023;46:A129-A129.
- Varghese B, Joseph CM, Al-Akkam AA, AL-Balawi RM, Swallmeh E, et al. Nurse’s experience working 12-hour shift in a tertiary level hospital in Qatar: A mixed method study. BMC Nurs. 2023;22(1):213.
[Crossref][Google Scholar][PubMed]
- Toffoli B, Tonon F, Giudici F, Ferretti T, Ghirigato E, et al. Preliminary study on the effect of a night shift on blood pressure and clock gene expression. Int J Mol Sci. 2023;24(11):9309.
[Crossref][Google Scholar][PubMed]
- Lesage FX, Berjot S, Deschamps F. Clinical stress assessment using a visual analogue scale. Occup Med. 2012;62(8):600-605.
[Crossref][Google Scholar][PubMed]
- Li Y, Scherer N, Felix L, Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PloS One. 2021;16(3):e0246454.
[Crossref][Google Scholar][PubMed]
- Tomes C, Schram B, Orr R. Relationships between heart rate variability, occupational performance and fitness for tactical personnel: A systematic review. Front Public Health. 2020;8:583336.
[Crossref][Google Scholar][PubMed]
- Tamrakar P, Pant SB, Acharya SP. Anxiety and depression among nurses in COVID and non‐COVID intensive care units. Nurs Crit Care. 2023;28(2):272-280.
[Crossref][Google Scholar][PubMed]
Citation: Integrating Heart Rate Variability and Psychometric Assessments to Evaluate Stress and Burnout in ICU Nursing Staff: A
Pilot Study ASEAN Journal of Psychiatry, Vol. 25 (7) September, 2024; 1-12.