Introduction
Substance use is a common condition and often
presents with psychotic symptoms. In fact, 7%-
25% of first episode psychosis is precipitated
by substance use [1]. Conversion rates from
Substance-Induced Psychotic Disorders (SIPD) to a Primary Psychotic Disorder (PPD) such as
schizophrenia vary with type of substance used.
Rates are highest (34%-50%) among cannabisinduced
psychotic disorder and lowest (5%)
among alcohol-induced psychotic disorder
[2-6]. Methamphetamine use can induce a
psychotic state known as Amphetamine-Induced Psychotic Disorder (AIPD) as defined by the
Diagnostic criteria in the fifth edition (DSM-5)
of the diagnostic and statistical manual of mental
disorders. There are an estimated 27 million
amphetamine users worldwide and approximately
2.3% of the North American population between
the ages of 15-64 have used amphetamines in the
past year [7]. It is estimated that as many as 40%
of amphetamine users experience AIPD [2].
Established risk factors for AIPD include a history
of a PPD, schizotypal and antisocial personality
disorders, family history of mental illness, and
methamphetamine dependence [8]. Conversion
rates from AIPD to a primary psychotic disorder
are in the range of 19%-40% [2,3,6,9,10]. There
are many Subjects (or is it Subjects-level) factors
that contribute in conversion from a SIPD to a
PPD (schizophrenia or schizoaffective disorder)
including a family history of schizophrenia in a
first degree relative, male gender, subjects living
in urban areas, an extended duration of untreated
psychosis, continued substance abuse after index
psychotic episode, younger age at the time of the
first episode of substance induced psychosis, and
having a preexisting diagnosis of either a substance
use disorder, personality disorder (specifically
schizotypal and antisocial), or an eating disorder
prior to the index psychotic episode [2,6,11].
Moreover, conversions may occur rapidly. In one
study, it has been shown that 50% of conversions
from SIPD to schizophrenia occur within 3.1 years
of the index substance induced psychotic episode
[6].
Treatment of Substance Use Psychotic Disorders
(SIPD) is evolving [12]. It is a recent diagnostic
addition in the DSM-IV and has fallen under
significant scrutiny [13]. Subjects presenting
psychotic in the context of substance abuse are
often diagnosed with AIPD and providers may
neglect to consider the presence of an underlying
primary psychotic disorder. Confirmation bias is
an issue may delay in antipsychotic treatment or
inaccurate Subjects advice that the symptoms will
resolve with cessation of drugs alone. This may
lead to suboptimal treatment of Subjects with SIPD
[12]. Additionally, the SIPD Subjects population
is often excluded from clinical trials resulting in
a paucity of data to guide clinicians for subjects’
management [14,15]. This is alarming because
AIPD Subjects suffer from severe symptoms,
higher rates of hospitalization, and are more likely
to attempt suicide than methamphetamine users
without psychotic features [16]. Furthermore, younger AIPD Subjects with an average age of
30.4 years and a history of requiring hospitalization
have unusually high mortality rates (>8%) within
6 years of hospitalization [9]. This is of particular
concern within the veteran population given
that the suicide rate is higher among veterans as
compared to the general population and suicide
rate is doubled among veterans with a diagnosis
of a substance use disorder [17,18]. Despite
alarmingly high rates of mortality within the AIPD
subjects population, treatment is often delayed
resulting in prolonged periods of psychosis and
a poor prognosis [5]. To date there are only few
studies conducted in the in the veteran population.
Given the elevated risk of suicide within the
veteran population this study was undertaken to
understand the demographic profile, incidence
of mental disorders, substance use trends and
associated psychotic disorders among subjects
with mental illness admitted to a National VA
Medical Center (VAMC).
Materials and Methods
Data base and study design
Veterans’ Health Administration’s Corporate Data
Warehouse (VHA-CDW) uses a unique identifier
to identify veterans across treatment episodes at
more than 1,400 VHA centers organized under 21
Veterans Integrated Service Networks (VISNs).
The VHA-CDW database contains veteran
health care information comprised of diagnostic,
laboratory, pharmacy, and other procedure related
data from various sources in the electronic health
record. VHA-CDW data and the VA Informatics
and Computing Infrastructure (VINCI) workspace
have been used widely for numerous studies of
clinical importance. Since we used VHA-CDW
and VINCI to extract data, consent has not been
necessary for this retrospective cohort study [19].
Study population
Mental health conditions, a composite measure
that included Psychosis, Manic-bipolar disorders,
PTSD, schizophrenia, depression and TBI all
defined by ICD-9 and ICD-10 according to
International Statistical Classification of Diseases
and Related Health Problems, Ninth and Tenth
Revision (ICD-9, ICD-10) codes, between
October 1, 1999, and February 27, 2022. The
study population consisted of 156,435 veterans
with MHC diagnosis (Group 2). We randomly
selected a total of 156,189 cases of admissions of similar gender, race, and age without any MHC
diagnosis (Group 1) during that period, balanced
for confounding factors such as age, race, sex,
smoking and Type 2 diabetes. The final study
groups comprise cases admitted to hospital with
and without various mental illnesses.
Data analysis
We used the date of first admission (first
occurrence in the data set) in the sample period
10/1/1999 through 02/27/2022 as the index time
point to differentiate pre-existing and new events
data and used a combination of standard SQL
accessible files such as ICD, lab, or drugs and free
text medical and administrative record searches
to collect information on conditions, medications,
and procedures.
Data were mainly used as categorical variables
and was analyzed by standard frequency tables
(chi sq and Odds ratios) using SAS (Guide 8.2)
was used for statistical analysis. Continuous
variables such as age are shown as Means (±
SD). Odds ratios (OR) were also calculated. A
Logistics procedure was used to initially evaluate
associations of multiple variables with the various
outcome variables. A greedy neighbor (nearest
neighbor) procedure was used as given by SAS
for the evaluation of all-cause mortality (death).
Principal outcomes were designated as number
of hospital admissions (1-9 or >10), suicide rate
(attempts/demise) and all-cause mortality among
two groups. Frequencies, means, and Odds ratios were calculated and are reported in the tables and
a p-value of <0.01 was deemed significant.
Ethics approval
This study (IRBNet #1663414) was approved
by the Kansas City VA Medical Center (FWA
00001481) Institutional Review Board (IORG
0000081) on March 17, 2022, and complies with
the declaration of Helsinki.
Results
Demographic characteristics of study population
We categorized principal demographics age groups (18-25, 26-35, 36-50, 51-65 and >65 years), race (American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or other Pacific Islander, white, White Not of Hispanic origin and declined to answer/ unknown), ethnicity (Hispanic/Latino, non- Hispanic/Latino and unknown/declined to answer) and marital status (single/never married, married, separated/divorced, widow/widower/widowed and unknown/missing).
As shown in Table 1, age had a measurable effect on prevalence of mental illness. The proportion of subjects with a diagnosis of mental illness increased up to the 50 years and declined in >50 years old subjects. Age groups (18-25, 26-35, 36- 50, 51-65 and >65 years) are shown. In general, older subjects did better (OR=0.81, p<0.001).
Table 1. Demographic characteristics of study population
| |
Group 1, subjects with
no Mental Health Conditions (MHC) diagnosis
N=156,189 |
Group 2 subjects with
MHC diagnosis
N=156,435 |
p-value Group 2 vs Group 1 |
| AGE groups, number (%) |
| 18-25 years |
125 (0.08%) |
172 (0.11%) |
- |
| 26-35 years |
6,388 (4.09%) |
9,730 (6.22%) |
- |
| 36-50 years |
24,537 (15.71%) |
33,555 (21.45%) |
- |
| 51-65 years |
80,422 (51.49%) |
74,760 (47.79%) |
- |
| Above 65 years |
44,701 (28.62%) |
38,201 (24.42%) |
- |
| ≥ 50 years |
44707 (28.62%) |
38,178 (24.42%) |
- |
| <50 years |
111,483 (71.38%) |
118257 (75.58%) |
<0.001 |
| Gender (sex), number (%) |
| Male |
147,769 (94.61%) |
146572 (93.7%) |
|
| Female |
8,421 (5.39%) |
9,855 (6.3%) |
<0.001 |
| Race characteristics-number (%) |
| American Indian/Alaska native |
1327 (0.85%) |
1455 (0.93%) |
- |
| Asian |
500 (0.32%) |
720 (0.46%) |
- |
| Black/African American |
63,788 (40.84%) |
62,089 (39.69%) |
- |
| Native Hawaiian/other pacific islanders |
984 (0.63%) |
1001 (0.64%) |
- |
| White |
82,218 (52.64%) |
84006 (53.7%) |
- |
| White not of Hispanic origin |
594 (0.38%) |
469 (0.3%) |
- |
| Unknown or declined to answer |
6,779 (4.34%) |
6695 (4.28%) |
- |
| White |
80,037 (51.24%) |
83,431 (53.33%) |
<0.001 |
| Others |
76,153 (48.76%) |
73,012 (46.67%) |
|
| Ethnicity characteristics, number (%) |
| Not Hispanic/Latino |
144,209 (92.33%) |
143482 (91.72%) |
- |
| Hispanic/Latino |
7403 (4.74%) |
9057 (5.79%) |
<0.001 |
| Unknown or declined to answer |
4576 (2.93%) |
3614 (2.31%) |
- |
| Marital status, number (%) |
| Single/never married |
38,204 (24.46%) |
41,721 (26.67%) |
- |
| Married |
28,176 (18.04%) |
27157 (17.36%) |
- |
| Separated/divorced |
83,483 (53.45%) |
81,925 (52.37%) |
- |
| Widow/widower/widowed |
5592 (3.58%) |
5350 (3.42%) |
- |
| Unknown/missing |
734 (0.47%) |
282 (0.18%) |
- |
| All-cause mortality, number (10%) |
| Alive |
1,02,380 |
1,12,023 |
<0.001 |
| Dead |
53,810 |
44,412 |
- |
|
Note: Numbers (%); Total subjects (percent).
|
Males were less frequently associated with mental diagnosis than females (OR=0.85, p<0.001). There was a difference in the prevalence of mental illness based on race (White vs other OR=0.92 p<0.001). Race and ethnicity were grouped (American Indian or Alaska native, Asian, black, or African American, native Hawaiian or other Pacific Islander, white, white not of Hispanic origin and declined to answer/unknown), ethnicity (Hispanic/Latino, Non-Hispanic/Latino and unknown/declined to answer) of interest, Hispanic were more likely to carry a diagnosis of mental illness (OR=1.28, p<0.001).
Marital status was examined (single/never married, married, separated/divorced, widow/widower/widowed and unknown/missing). A great majority of subjects in the study were divorced or separated. About 18% were married and about 25% had never been married of interest, death during study period was less common (OR=0.740, p<0.001) in mental illness group compared to control group.
Distribution of various MHC diagnoses
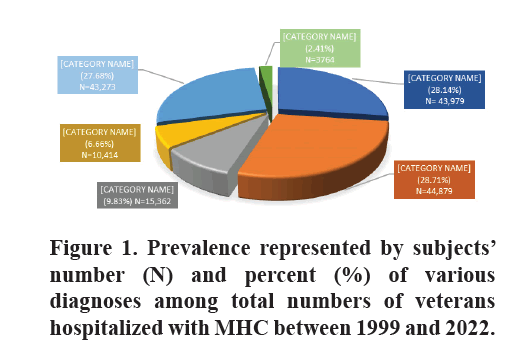
As shown in Figure 1, psychosis, manic-bipolar and PTSD were most common diagnosis at 28% each followed by schizophrenia (9.83%) and depression (6.66%). TBI was uncommon at 2.4% of cases. Our analysis did not exclude any cases from any category where there was overlap as the primary condition could not always be identified.
Frequency and types of substances used
Overall drugs use was very frequent in Group 2-MHC diagnosis (OR 11.1). There were notable differences for the types of drugs used. Barbiturates (OR 4.9), PCP (OR 5.0), and Cocaine (OR 5.2) use increased to a similar degree. Amphetamines (OR 9.4), Cannabis (OR 10.5) and Codeine (OR 13.9) were all increased even more strongly and a monumental increase in use of Morphine (OR 38.6) and Fentanyl (OR 57.9) was found in subjects with MHC.
As shown in Table 2, subjects with MHC diagnosis (Group 2) were significantly associated with an overall increase in substance use as compared to Group 1-no-MHC (11.98% vs 1.37%). The most abused substance was amphetamines (2.67% vs 0.29%) followed by cannabis (2.3% vs 0.23%), codeine, morphine, and cocaine. These were all at least two times as common as barbiturates or fentanyl. PCP use was uncommon among these subjects.
Table 2. Substances use frequency among subjects with and without Mental Health Conditions (MHC) diagnosis.
| |
Group 1 no MHC 156189 |
Group 2 MHC 156435 |
Odds ratio Group 2 vs Group 1 |
p-value Group 2 vs Group 1 |
| Drug users N (%) |
2134 (1.37%) |
18,744 (11.98%) |
11.1 |
<0.0001 |
| Amphetamine |
453 (0.29%) |
4179 (2.67%) |
9.4 |
<0.0001 |
| Barbiturates |
406 (0.26%) |
1927 (1.23%) |
4.9 |
<0.0001 |
| Cannabis |
359 (0.23%) |
3617 (2.31%) |
10.5 |
<0.0001 |
| Cocaine |
513 (0.33%) |
2650 (1.69%) |
5.2 |
<0.0001 |
| Codeine |
222 (0.14%) |
3051 (1.95%) |
13.9 |
<0.0001 |
| Fentanyl |
13 (0.01%) |
750 (0.48%) |
57.5 |
<0.0001 |
| Morphine |
52 (0.03%) |
1987 (1.27%) |
38.6 |
<0.0001 |
| PCP |
116 (0.07%) |
583 (0.37%) |
5 |
<0.0001 |
|
Note: Numbers as (percent) of total subjects in Group1 (control) and Group 2 (MHC); p-value represents significance when compared Group 2 vs Group 1.
|
Primary and drug-induced psychosis among veterans with mental health conditions
As shown in Table 3, about 28% (N=43,979) of 156,435 subjects with mental illness in this study carried a psychosis diagnosis of which majority were non-substance users (88.1%, N=38,710). Among 11.9% substance users (N=5269) with psychosis, only 1,174 subjects used amphetamine resulting in an Amphetamine Induced Psychotic Disorder (AIPD) rate of 22.28%. Psychosis among other substance users including cannabis, codeine, morphine, cocaine, barbiturates, fentanyl, and PCP persisted in 4,095 subjects resulting in Substance abuse related Psychosis Disorder (SIPD) rate of 77.72%.
Table 3. Amphetamine-Induced Psychosis Disorder (AIPD) vs other Substances-Induced Psychosis Disorder (SIPD) among subjects diagnosed with psychosis.
| Total veterans with MHC N=156,435 |
| Veterans with Psychosis DX N=43,979 (28.14%) |
| Substance users, N=5,269 (11.98%) |
Non-substance users N=38,710 (88.01%) |
| Amphetamine users, N= 1,174 |
Other substance users N=4095 |
| AIPD rate 22.28% |
SIPD rate 77.72% |
|
Note: Numbers as (percent) of total subjects in the category; AIPD and SIPD rate in % is calculated by dividing numbers of amphetamine and other substances users by the number of substance users with psychosis diagnosis.
|
Frequency of hospitalization, suicide attempts and suicide death
Principle outcome examined included >10 hospitalization, suicide, attempts and suicide death. As shown in Table 4, frequency of hospitalization (>10 admissions) was significantly higher (p-value <0.001) in population with mental illness, Group 2 (52.95%) as compared to no mental illness Group 1 (47.11%) with an OR=1.22. Similarly, rate of suicide rate, attempts and death was also significantly higher (p<0.0001) in mental illness Group 2 as compared to no mental illness Group 1.
Table 4. Comparison of outcomes among subjects with and without MHC
| Measured outcome |
Group 1 control (no-MHC)
156,189 |
Group 2 MHC diagnosis
156,435 |
Odds ratio Group 2 vs Group 1 |
p-value Group 2 vs
group 1 |
| >10 admissions |
73,581 (47.11%) |
81,419 (52.05%) |
1.22 |
<0.0001 |
| Suicide |
3,972 (2.54%) |
58,012 (37.08%) |
23.32 |
<0.0001 |
| Attempt |
2,644 (1.69%) |
43,035 (27.51%) |
57.5 |
<0.0001 |
| Suicide |
1,328 (0.85%) |
14,698 (9.40%) |
38.6 |
<0.0001 |
|
Note: Numbers as (percent) of total subjects in Group 1 (control) and Group 2 (MHC); p-value represents significance when compared Group 2 vs Group 1.
|
Discussion
Demographic characteristics of our study
population demonstrated that mental illness
diagnosis was less frequently associated with
males than females (OR=0.85, p<0.001). These
findings parallel global statistics. The agestandardized
disability-adjusted life-years rate for
mental disorders, prevalence and incidence rates
of common mental disorders, specifically affective
disorders, such as anxiety and depression, is greater
in females than males [20,21]. We found that
overall mortality was less common (OR=0.740,
p<0.001) in mental illness group compared to
control group. This correlates with the findings
of the systematic analysis for the Global Burden
of Disease Study 2019, which concluded that
estimated years of life lost for mental disorders
were low and do not reflect premature mortality
in individuals with mental illness [20]. Veterans
of Hispanic origins were more likely to carry a
diagnosis of mental illness (OR=1.28, p<0.001).
Our data and published reports suggest a need to
do additional epigenetic and sociocultural research
in the Hispanic population [22].
We found that substance abuse was significantly
higher in the mental illness group (11.98%)
compared to the control group (1.37%, (OR=11.1).
Co-occurring Substance Use Disorders (SUD) with
Mental Disorders is a well-known phenomenon,
frequently referred as a dual diagnosis, which is
highly prevalent and represents a serious national
health problem. Unfortunately, it is often underdiagnosed
and therefore, poorly treated. In a
nationally representative U.S sample, dually
diagnosed adults are estimated to represent 17.8%
of the 75.6 million adults diagnosed with SUD and
Mental disorder [23].
We observed a monumental increase in abuse of
morphine (OR=38.6) and fentanyl (OR-57.9) by
48 and 42 times, respectively, among subjects with
mental illness when compared with hospitalized
adults without concurring mental illness. It is well
known that a dual diagnosis is especially prevalent
among adults with the Opioid Use Disorder
(OUD) and that it increases the risk for morbidity
and mortality. For instance, 24.5% of adults with
OUD and recent mental illness in the past year
and 29.6% of adults with OUD and serious mental illness reported receiving services for both mental
health and substance use treatment [24]. This
is alarming because opioid abuse in the US has
reached an epidemic status. The alarming increase
in fentanyl abuse found in our study corresponds
with the current course of the US opioid crisis.
Three main causes for the opioid epidemic are:
• Increase in prescription of opioids,
• Drug use, and
• Access to illicitly manufactured fentanyl.
Centers for disease control and prevention
statistics estimated 500,000 opioid associated
deaths between 1996 and 2019.
While death related to the opioid drug overdose
started to decline in 2017, Fentanyl use associate
deaths continue to increase [25].
Use of amphetamine among veterans with mental
illness is higher than estimated use among 15-64
years old North American population. We detected
that amphetamines (OR=9.4), cannabis (OR=10.5)
and codeine (OR=13.9) abuse was 9.2 to 13.92
times more frequently noted in the MHC group.
Moreover, amphetamine was the most frequently
used substance (2.67%), followed by cannabis
(2.3%), codeine, morphine, cocaine, barbiturates,
fentanyl, and PCP in the mental illness group. Our
findings correlate with both nation and worldwide
trends, showing that synthetic drugs, represented
by methamphetamine, have become the most
abused drugs in the world and have surpassed
traditional drugs of abuse (including opioids).
The rates of stimulant use disorders, including
methamphetamine, and stimulant-related overdose
and mortality is steadily increasing in the USA
[26-29].
We observed that Amphetamine Induced Psychotic
Disorder (AIPD) presented in 22.28% whereas
other Substance (cannabis, codeine, morphine,
cocaine, barbiturates, fentanyl, and PCP) Induced
Psychotic Disorder (SIPD) presented in 77.72%.
Psychosis has been described in the medical
literature as a well-known complication of longterm
methamphetamine use since after the Word
War II. Epidemiologic studies provide different
opinions regarding the prevalence of AIPD [30].
One meta-analysis of seventeen studies showed a
composite event rate of 36.5%. Overall, difference
in prevalence of AIPD varies from 13% in the
USA to 50% in Asia that can be explained by the
potency and purity of methamphetamines used in different geographic locations [31].
The time elapsed from the initial substance use to
developing AIPD varies from a few weeks to years.
It is influenced by the frequency of consumption,
dose of the substance, route of administration
(intravenous, oral, inhalation), and individual
vulnerability to psychosis. Early consumption of
amphetamines initially induces psychotomimetic
effects, to include euphoria, feelings of increased
concentration and stimulation. Continuous use
of methamphetamines induces pre-psychotic
delusional moods followed by overt psychotic
state manifesting with delusions and hallucinations
[32].
In our study 11.98% of veteran-subjects with
psychosis diagnosis used substance. Psychosis
among amphetamine and other substance users
presented at higher rate among subjects with mental
illness. The most prevalent AIPD symptoms are
persecutory delusion (82%), auditory hallucination
(70.3%), and delusion of reference (57.7%),
visual hallucination (44.1%), grandiosity delusion
(39.6%) and jealousy delusion (26.1%). AIPD
may be accompanied by severe violent behavior
warranting clinical intervention to prevent harm
to subjects and society. Tactile hallucinations are
more so frequent among subjects using higher
daily doses of the drug and frequently described
as parasites crawling under subject’s skin
(formication, “meth mites”).
Chronic methamphetamine use induces
neuroinflammation, ischemia, oxidative stress,
and direct neurotoxicity leading to degeneration
processes. It may unmask or expedite the
development of schizophrenia in first-degree
relatives of subjects with schizophrenia,
emphasizing the importance of differentiating
AIPD from schizophrenia. Higher prevalence
of visual and tactile hallucinations was reported
among subjects with AIPD vs schizophrenia,
while delusion patterns were similar in both
groups. Subjects with AIPD have less “negative”
psychotic symptoms (i.e., social withdrawal,
blunted affect, disorganization, etc.,) and similar
levels of “positive” symptoms (i.e., hallucinations,
paranoid delusions) compared with schizophrenic
subjects [32,33].
The large number of drug reactions and side
effects would be expected to lead to increased
use of medical services and complications.
Indeed, we found that a diagnosis of mental
illness was significantly associated with higher(>10) admission rates (OR=1.22), suicide rate
(OR=23.3), suicide attempts (OR=57.5), and
suicide death (OR=38.6). Suicide is more prevalent
among veterans compared with the general US
population. Data published by the US department
of Veterans affairs in 2016 showed that veteran
suicide rates were 1.5 times higher than among
non-veterans. Our data coincide with the findings
that mental illness significantly increases the risk
of suicide in veterans, in addition to other risk
factors, such as older age, male gender, substantial
medical comorbidities, substance abuse etc., [34-36]. Female veterans with substance use disorders
are at particularly elevated risk for suicide [37].
Moreover, approximately 30% of completed
suicides and 20% of deaths resulting from high risk
behavior were attributed to substance use,
according to the study conducted on military
personnel [38,39].
Both suicide rates (37.08%) and substance use
(11.98%) were significantly higher in the mental
illness group compared to control group (2.54%
and 1.37% correspondingly). Substance use has
been identified as a strong risk factor for suicidal
behavior among US Veterans [38]. Amphetamine
was the most used substance followed by
cannabis in the studied mental illness group.
The incidence of overdose-induced deaths due
to psycho-stimulants other than cocaine (largely
methamphetamine) is on significant rise. Cannabis
use has also been indicated as a risk factor for
suicide in veterans. Logistic regression models
indicated that cannabis use was associated with
past year suicidal ideation and elevated risk for
suicidal behavior. These findings included a
concerning association between cannabis use and
suicide risk in Gulf War veterans [40].
Increasingly common use of stimulants with
synthetic opioids, such as fentanyl and its
analogies and surge in amphetamine use and
AIPD among veterans with mental illness in
the light of documented high rates of mortality
associated with amphetamine use and substanceinduced
psychosis is underestimated and warrants
immediate attention to this mental health
emergency. Keeping in mind the deadly risks
associated with it, methamphetamine has become
“America’s most dangerous drug”. Stimulantrelated
deaths involving psycho-stimulants other
than cocaine (largely methamphetamine) are on
the rise in the United States. Psycho-stimulantrelated
mortality has progressively increased
5-fold from 2012 to 2018 [29,36].
Unfortunately, there are no FDA-approved
medications for treating either AIPD or
methamphetamine use disorder. Most medications
evaluated for methamphetamine/amphetamine use
disorder have not shown a statistically significant
benefit. However, there is low-strength evidence
that Methylphenidate may reduce amphetamine/
methamphetamine use.
Numerous Randomized Controlled Trials (RCTs)
investigated over 20 potential pharmacotherapies.
Methylphenidate, Bupropion, Modafinil, and
Naltrexone demonstrated limited evidence
of benefit for reducing amphetamine use.
Dexamphetamine has benefit on treatment
retention, but not for reducing amphetamine
use. Based on moderate strength evidence,
antidepressants as a class, to include SSRIs, have
not shown statistically significant effect on either
abstinence or treatment retention [41,42].
Methamphetamine triggers neurotoxicity,
oxidative change, neuroinflammation, induces
cell death cascade, and degenerative loss of
dopaminergic neurons in the brain, which
contributes to the higher risks of developing
Parkinsonism syndrome and Parkinson’s disease
itself among methamphetamine users [43].
Therefore, when treating AIPD, clinicians should
keep in mind that these subjects are at increased
risks of extrapyramidal movement complications,
if treated with the first-generation antipsychotics,
such as Haloperidol. Consequently, secondgeneration
antipsychotics maybe a preferable class
to address psychotic symptoms of AIPD. Subjects
diagnosed with substance induced psychotic
disorder require close follow up and treatment
with psychotropic medications.
Conclusion
In conclusion, our results call for action to increase awareness among VHAs and general practicing clinicians to address the surge in amphetamine use and related mortality, seek evidence-based prevention strategies, and treatment interventions for the amphetamine use associated disorder including AIPD. Further research is urgently needed to identify successful public health approaches targeting Methamphetamine abuse epidemic and to develop effective clinical interventions and relapse prevention strategies.
Our findings underscore the importance of considering demographic factors such as age, gender, race, and service-related characteristics in understanding the complex landscape of mental health among veterans. Furthermore, the link between substance use and psychotic disorders among this population highlights the need for integrated screening, prevention, and treatment approaches that address both mental health and substance use disorders concurrently.
Limitations of our study include
• False-positive or false-negative Urine Drug Screens (UDS) for amphetamine might have occurred in small number of subjects.
• UDS amphetamines detection could have included prescription stimulants for ADHD, narcolepsy, off-label treatment for major depressive disorder, weight-loss medication, etc., and
• Initial diagnosis of AIPD could have overlapped with unmasked symptoms of first onset of psychosis, schizophrenia, or schizophrenia-like presentation secondary to poly substance use, including highly potent synthetic cannabinoids.
Acknowledgements
This work was supported by the resources from
both Kansas City VA medical center and Midwest
Veterans biomedical research foundation.
Disclosures
The contents of this article are those of authors and
do not necessarily reflect the position and policy
of the Department of Veterans Affairs. All authors’
participants have given consent for their data to
be used in the research. The data that support
the findings of this study are available from the
corresponding author, (RS), upon reasonable
request.
References
- Regier DA, Kuhl EA, Kupfer DJ. The DSM‐5: Classification and criteria changes. World Psychiatry. 2013;12(2):92-98. [Crossref][Google Scholar][PubMed]
- Murrie B, Lappin J, Large M, Sara G. Transition of substance-induced, brief, and atypical psychoses to schizophrenia: A systematic review and meta-analysis. Schizophr Bull. 2020;46(3):505-516. [Crossref][Google Scholar][PubMed]
- Niemi-Pynttäri JA, Sund R, Putkonen H, Vorma H, Wahlbeck K, et al. Substance-induced psychoses converting into schizophrenia: A register-based study of 18,478 Finnish inpatient cases. J Clin Psychiatry. 2013;74(1):20155. [Crossref][Google Scholar][PubMed]
- Shah D, Chand P, Bandawar M, Benegal V, Murthy P. Cannabis induced psychosis and subsequent psychiatric disorders. Asian J Psychiatr. 2017;30:180-184. [Crossref][Google Scholar][PubMed]
- Jeppesen P, Petersen L, Thorup A, Abel MB, Øhlenschlaeger J, et al. The association between pre-morbid adjustment, duration of untreated psychosis and outcome in first-episode psychosis. Psychol Med. 2008;38(8):1157-1166. [Crossref][Google Scholar][PubMed]
- Starzer MS, Nordentoft M, Hjorthøj C. Rates and predictors of conversion to schizophrenia or bipolar disorder following substance-induced psychosis. Am J Psychiatry. 2018;175(4):343-350. [Crossref][Google Scholar][PubMed]
- Substance abuse and mental health services administration. 2021.
- Glasner-Edwards S, Mooney LJ. Methamphetamine psychosis: Epidemiology and management. CNS Drugs. 2014;28:1115-1126. [Crossref][Google Scholar][PubMed]
- Kittirattanapaiboon P, Mahatnirunkul S, Booncharoen H, Thummawomg P, Dumrongchai U, et al. Long‐term outcomes in methamphetamine psychosis patients after first hospitalisation. Drug Alcohol Rev. 2010;29(4):456-461. [Crossref][Google Scholar][PubMed]
- Alderson HL, Semple DM, Blayney C, Queirazza F, Chekuri V, et al. Risk of transition to schizophrenia following first admission with substance-induced psychotic disorder: A population-based longitudinal cohort study. Psychol Med. 2017;47(14):2548-2555. [Crossref][Google Scholar][PubMed]
- Björkenstam E, Björkenstam C, Hjern A, Reutfors J, Bodén R. A five year diagnostic follow-up of 1840 patients after a first episode non-schizophrenia and non-affective psychosis. Schizophr Res. 2013;150(1):205-210. [Crossref][Google Scholar][PubMed]
- Van Boekel LC, Brouwers EP, Van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. [Crossref][Google Scholar][PubMed]
- Mathias S, Lubman DI, Hides L. Substance-induced psychosis: A diagnostic conundrum. J Clin Psychiatry. 2008;69(3):358-367. [Crossref][Google Scholar][PubMed]
- Weibell MA, ten Velden Hegelstad W, Johannessen JO. Substance-induced psychosis: Conceptual and diagnostic challenges in clinical practice. InNeuropathology of Drug Addictions and Substance Misuse 2016:50-57. [Google Scholar]
- Fusar-Poli P, Cappucciati M, Bonoldi I, Hui LC, Rutigliano G, et al. Prognosis of brief psychotic episodes: A meta-analysis. JAMA psychiatry. 2016 Mar 1;73(3):211-20. [Crossref][Google Scholar][PubMed]
- Glasner-Edwards S, Mooney LJ, Marinelli-Casey P, Hillhouse M, Ang A, et al. Clinical course and outcomes of methamphetamine-dependent adults with psychosis. J Subst Abuse Treat. 2008;35(4):445-450. [Crossref][Google Scholar][PubMed]
- Blow FC, Bohnert AS, Ilgen MA, Ignacio R, McCarthy JF, et al. Suicide mortality among patients treated by the veterans health administration from 2000 to 2007. Am J Public Health. 2012;102(S1):S98-104. [Crossref][Google Scholar][PubMed]
- Ilgen MA, Bohnert AS, Ignacio RV, McCarthy JF, Valenstein MM, et al. Psychiatric diagnoses and risk of suicide in veterans. Arch Gen Psychiatry. 2010;67(11):1152-1158. [Crossref][Google Scholar][PubMed]
- VA Informatics and Computing Infrastructure (VINCI). 2024.
- GBD. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: A systematic analysis for the global burden of disease study 2019. Lancet Psychiatry. 2022;9(2):137-150. [Crossref][Google Scholar][PubMed]
- Shimamoto A, Rappeneau V. Sex-dependent mental illnesses and mitochondria. Schizophr Res. 2017;187:38-46. [Crossref][Google Scholar][PubMed]
- Alarcón RD, Parekh A, Wainberg ML, Duarte CS, Araya R, et al. Hispanic immigrants in the USA: Social and mental health perspectives. Lancet Psychiatry. 2016;3(9):860-870. [Crossref][Google Scholar][PubMed]
- Jegede O, Rhee TG, Stefanovics EA, Zhou B, Rosenheck RA. Rates and correlates of dual diagnosis among adults with psychiatric and substance use disorders in a nationally representative US sample. Psychiatry Res. 2022;315:114720. [Crossref][Google Scholar][PubMed]
- Jones CM, McCance-Katz EF. Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug Alcohol Depend. 2019;197:78-82. [Crossref][Google Scholar][PubMed]
- Gardner EA, McGrath SA, Dowling D, Bai D. The opioid crisis: Prevalence and markets of opioids. Forensic Sci Rev. 2022;34(1):43-70. [Google Scholar][PubMed]
- Courtney KE, Ray LA. Methamphetamine: An update on epidemiology, pharmacology, clinical phenomenology, and treatment literature. Drug Alcohol Depend. 2014;143:11-21. [Crossref][Google Scholar][PubMed]
- Fogger SA. Methamphetamine use: A new wave in the opioid crisis? J Addict Nurs. 2019;30(3):219-223. [Crossref][Google Scholar][PubMed]
- Ciccarone D, Shoptaw S. Understanding stimulant use and use disorders in a new era. Med Cli North Am. 2022;106(1):81-97. [Crossref][Google Scholar][PubMed]
- Ciccarone D. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr Opin Psychiatry. 2021;34(4):344-350. [Crossref][Google Scholar][PubMed]
- Lecomte T, Dumais A, Dugre JR, Potvin S. The prevalence of substance-induced psychotic disorder in methamphetamine misusers: A meta-analysis. Psychiatry Res. 2018;268:189-192. [Crossref][Google Scholar][PubMed]
- Ujike H, Sato M. Clinical features of sensitization to methamphetamine observed in patients with methamphetamine dependence and psychosis. Anna N Y Acad Sci. 2004;1025(1):279-287. [Crossref][Google Scholar][PubMed]
- Fasihpour B, Molavi S, Shariat SV. Clinical features of inpatients with methamphetamine-induced psychosis. J Ment Health. 2013;22(4):341-349. [Crossref][Google Scholar][PubMed]
- Edinoff AN, Kaufman SE, Green KM, Provenzano DA, Lawson J, et al. Methamphetamine use: A narrative review of adverse effects and related toxicities. Health Psychol Res. 2022;10(3). [Crossref][Google Scholar][PubMed]
- Inoue C, Shawler E, Jordan CH, Moore MJ, Jackson CA. Veteran and military mental health issues. 2023. [Google Scholar][PubMed]
- Barbic D, Whyte M, Sidhu G, Luongo A, Chakraborty TA, et al. One-year mortality of emergency department patients with substance-induced psychosis. PLoS One. 2022;17(6):e0270307. [Crossref][Google Scholar][PubMed]
- Han B, Compton WM, Jones CM, Einstein EB, Volkow ND. Methamphetamine use, methamphetamine use disorder, and associated overdose deaths among US adults. JAMA Psychiatry. 2021;78(12):1329-1342. [Crossref][Google Scholar][PubMed]
- Chapman SL, Wu LT. Suicide and substance use among female veterans: A need for research. Drug and Alcohol Dependence. 2014;136:1-0. [Crossref][Google Scholar][PubMed]
- Na PJ, Nichter B, Hill ML, Kim B, Norman SB, et al. Severity of substance use as an indicator of suicide risk among US military veterans. Addict Behav. 2021;122:107035. [Crossref][Google Scholar][PubMed]
- Bohnert KM, Ilgen MA, Louzon S, McCarthy JF, Katz IR. Substance use disorders and the risk of suicide mortality among men and women in the US Veterans health administration. Addiction. 2017;112(7):1193-1201. [Crossref][Google Scholar][PubMed]
- Grove JL, Kimbrel NA, Griffin SC, Halverson T, White MA, et al. Cannabis use and suicide risk among gulf war veterans. Death Stud. 2023;47(5):618-623. [Crossref][Google Scholar][PubMed]
- Lee NK, Jenner L, Harney A, Cameron J. Pharmacotherapy for amphetamine dependence: A systematic review. Drug Alcohol Depend. 2018;191:309-37. [Crossref][Google Scholar][PubMed]
- Chan B, Freeman M, Kondo K, Ayers C, Montgomery J, et al. Pharmacotherapy for methamphetamine/amphetamine use disorder-a systematic review and meta‐analysis. Addiction. 2019;114(12):2122-2136. [Crossref][Google Scholar][PubMed]
- Jayanthi S, Daiwile AP, Cadet JL. Neurotoxicity of methamphetamine: Main effects and mechanisms. Expe Neurol. 2021;344:113795. [Crossref][Google Scholar][PubMed]
Citation: Demographic Profile, Substance use Trends and Associated Psychotic Disorders among Veterans with Mental Health
Conditions: A Retrospective Cohort Study of Us Veterans ASEAN Journal of Psychiatry, Vol. 25 (7) July, 2024; 1-11.