Introduction
Health anxiety/hypochondriasis is a significant new diagnosis that is growing in prevalence due to evolving health perceptions, especially with the emergence of the new worldwide COVID-19 pandemic. To the extent that they are frequently over-investigated, health anxiety leads people to
seek unnecessary medical consultations [1]. Health anxiety is characterized as obsessive and repetitive health-related behaviors, exacerbated by severe misinterpretation of bodily symptoms. It involves the fear of having a serious medical condition that continues through rigorous medical examination and frequent reassurance that the patient does not suffer from the disease feared [2].
Therefore, the advent of COVID-19, a global public health emergency that has adversely affected many individuals worldwide, has raised health anxiety. More than 26.1 million people were affected by the pandemic, with 864K confirmed deaths in 202 countries as of 3 September 2020. Health anxiety comprises two primary elements, Illness Anxiety Disorder (IAD) and somatic symptoms, which were commonly known as somatoform disorders in the DSM-IV-TR, according to the Diagnostic and Statistical Manual of Psychiatric Disorders (DSM-V) [3,4,5]. IAD patients do not have medical disorders reported, but they have increased body sensations, and they are still highly nervous about the prospect of an undiagnosed disease [6].
The use of the internet for medical information search leads to cyberchondriasis, which denotes the relation between cyber and hypochondriasis. The concept is used to clarify the detrimental consequences of the internet's excessive search for health information [7,8]. More recently, cyberchondria refers to the underlying health anxiety and non-reassurability as a pattern of excessive and persistent internet symptom- checking activity [8]. Approximately 89% of
American [7,9] and 75% of foreign site users [10] are searching for health information online. Patients carry out Google search and self- management searches, which are currently referred to as "Dr. Google" [11].
Dr. Google, 'Health Googling,' which involves an excessive online search for health information, has many advantages; it offers a vast volume of information accessible to internet users; it enables users to search for health information on the internet at a low cost; and the internet can also secure interactions with other patients and social support [8,9,12]. On the contrary, cyberchondria may include digital divisions that increase health disparities, often misleading, inaccurate, incorrect or out-of-date web-based health information [10,13,14]. Furthermore, overuse of the internet for health information may exaggerate health anxiety [12,15-18]. The overuse of internet to find medical information exaggerates health anxiety. It is argued that substantial amounts of individuals with medical records may succeed to get medical information online, others are confused. Therefore, people assume that much of the online medical
information given by online medical websites is inaccurate [19-21].
Furthermore, the extent of health anxiety can be explained by the Health Locus of Control (HLC), one of the most important factors associated with the perception of pain individuals experience. Individuals in their perception of control of life events fall into two main categories; individuals with the Internal Control Locus (ILC) and others with the External Control Locus (ELC). Individuals with ILC believe that they have full control of life events; it may/may not happen because they want it [22]. On the other hand, individuals with ELC fall into two subgroups; chance control, which includes the belief that life events are controlled by factors such as luck or fate and by others, including the belief that others control events such as health professionals, relatives and others [23].
Research on the impacts of COVID-19 anxiety has shown that individuals' anxiety, depression are predictors of health anxiety throughout the coronavirus pandemic. Gender variations may also be detected, female participants residing in urban locations and had previous psychiatric disease history were seen as subject for risk factors such as anxiety, depression and health stress [24]. Additionally, elevated levels of COVID-19 health anxiety have led people to seek medical advice online. Liu views that majority of people usually searches for information in online platforms associated with COVID-19 anxiety, this activity encouraged individuals to practice preventive behaviors either in direct or indirect manner [25].
Online information seeking behavior influences people' threat and coping perceptions, it relates to their self-isolation intention. Therefore, using social media as a source of information raised both cyberchondria and data overload [26]. In addition, COVID-19 information seeking behavior correlates with anxiety symptoms among parents in Bahraini society. During COVID-19 outbreak in Bahrain, about 18% of responding parents had moderate-to-severe anxiety symptoms (score ≥10 on GAD-7) [27]. Studies have revealed that online information seeking has adverse impacts on individuals’ health anxiety. Social media has a significant impact on spreading fear and panic related to the COVID-19 outbreak in Iraqi Kurdistan, with a potential negative influence on people’s mental health and psychological well- being. It has been shown that the majority of youths aged 18-35 years are facing psychological anxiety [27].
Therefore, COVID-19 anxiety was linked to people' health locus of control, it's shown that people with considerable anxiety due to the pandemic are hyper-vigilant so as to save their lives during the outbreak [28]. Whereas, certain studies revealed that there is no substantial connection between health locus of control (internal and external) and health behavior [29]. Additionally, the mediating impact of health anxiety in the relationship between functional somatic symptoms and illness behavior has been evident from Chinese patients with depression. It was revealed that health anxiety plays a somewhat significant function in the connection between functional somatic symptoms and illness behavior [30].
Aims of the study
Until now, there has been many researches that have dealt with the relevant factors associated with COVID-19 anxiety, yet there is a dearth of studies conducted in the Middle East and Gulf states. In particular, there are hardly any studies on the COVID-19 pandemic anxiety in relation with health anxiety, overuse of internet use to search for medical information (cyberchondria), and health locus of control in the Arab region. During pandemics such as COVID-19, it was presumed that individuals with pre-existing health anxiety or hypochondriasis would be particularly vulnerable to anxiety and adverse behaviors, but there is little empirical research on this [31].
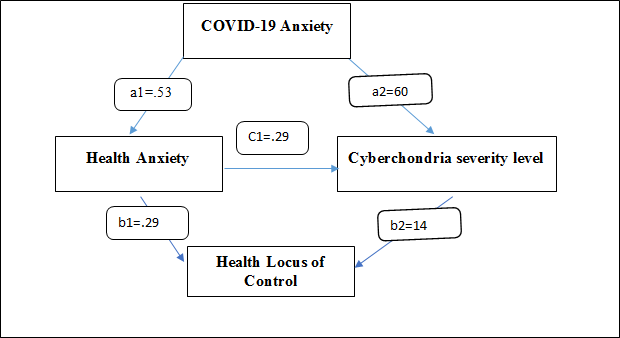
The aim of this study was to investigate the links between health anxiety, cyberchondria, and health locus of control during COVID-19 pandemic. It was hypothesized that COVID-19 anxiety mediates the relationship between health anxiety, cyberchondria severity and health locus of control.
Hypothesis
1. There are significant differences in the respondents’ levels of COVID-19 anxiety, health anxiety level and cyberchondria severity levels.
2. High levels of COVID-19 anxiety are associated with increased levels of cyberchondria severity, health anxiety, and health locus of control among study sample.
3. COVID-19 anxiety syndrome mediates the relationship between health anxiety, cyberchondria severity and health locus of control.
Methods
Participants and Procedure
Between 15 and 30 May 2020, individuals from 15 MENA & Gulf states were recruited via press releases (print, online, local and national), social media (e.g. Facebook and WhatsApp) email distribution lists of students, academics and people residing in MENA and Gulf states. The study tools have been designed to be distributed, completed and submitted online due to social distance procedures. As per WHO’s Situation Report of 25 September 2020, all countries in the Arab region have reported COVID-19 cases. Yemen was the last, reporting its first case on 9 April 2020. Most countries in the region have national rapid response for timely investigation and response to public health threats. However, staff in these national teams will require updated training to investigate and respond to the new coronavirus.
A total of 573 individuals in the MENA and Gulf Arab states participated in the current study. e demographic characteristics, employment status and internet exposure in the time of the pandemic were reported in Table 1. The majority of the sample is between 30 and 60 years of age, female participants are more than males, Egyptian citizens represent the majority of the sample, married individuals constitute the majority, and individuals with average annual income are the majority of the sample. In addition, the majority are individuals who spend 2-4 hours a day using the Internet and most of them are employed individuals. Specifically, 57.6 % of the sample was of female participants and 51.0 % of the study sample is married. As regards their socio- economic level, 70.3% of the total study sample is of average annual income, 27.4 % are above average, while 2.3% are below average. Most participants reported working during the COVID-
19 pandemic (55.5%) and 53.1% reported using the internet for 2 to 4 hours a day. The majority of the time spent online was spent searching for information and news about the COVID-19 pandemic, while 26.9% spent 4 to 8 hours a day surfing the internet.
| Demographic characteristics |
N |
% |
| Respondent nationality |
|
|
| Egyptian |
137 |
23.90% |
| Algerian |
63 |
11.00% |
| Syrian |
56 |
9.80% |
| Yemeni |
52 |
9.10% |
| Iraqi |
42 |
7.30% |
| Kuwaiti |
34 |
5.90% |
| Palestine |
33 |
5.80% |
| Lebanon |
32 |
5.60% |
| UAE |
26 |
4.50% |
| Libya |
26 |
4.50% |
| Bahrain |
23 |
4.00% |
| Jordan |
15 |
2.60% |
| KSA |
14 |
2.40% |
| Morocco |
10 |
1.70% |
| Oman |
10 |
1.70% |
| Gender |
|
|
| males |
243 |
42.40% |
| females |
330 |
57.60% |
| Marital status |
|
|
| Single |
256 |
44.70% |
| Married |
292 |
51.00% |
| Divorced |
19 |
3.30% |
| Widower |
6 |
1.00% |
| Socio- economic level |
|
|
| Below average |
13 |
2.30% |
| average |
403 |
70.30% |
| Above average |
157 |
27.40% |
| Time spent online |
|
|
| Less than an hour |
24 |
4.20% |
| 2-4 hours |
304 |
53.10% |
| 5-8 hours |
154 |
26.90% |
| More than 8 hours |
91 |
15.90% |
| Employment status |
|
|
| working |
318 |
55.50% |
| Not working |
255 |
44.50% |
Table 1. Demographic characteristics and current COVID-19 characteristics of the study sample (n=573).
The study protocol was approved by the local ethics committee of the Department of Psychology & Mental Health.
Measures
The Cyberchondria Severity Scale (CSS): The Cyberchondria Severity Scale (CSS) [32] comprised 33 items that assess cyberchondria. Scale items were translated from English into Arabic and back-translated into English again by two independent bilingual psychologists’ expert in the field. Participants were asked to rate the frequency of each item on Likert 5-point scale (1=never to 5=always). The CSS comprised five subscales, namely, “compulsion” (8 items e.g. researching symptoms or perceived medical conditions online interrupts my online leisure activities), “distress” (8 items, e.g. I have trouble relaxing after researching symptoms or perceived medical conditions online), “excessiveness” (8 items, e.g. I read different web pages about the same perceived condition), “reassurance” (6 items,
e.g. I discuss my online medical findings with my GP/health professional), and “mistrust of medical professional” (3 items to be reversed, which were retained to assess participants’ attitudes towards medical system during the pandemic). Higher scores on the scale indicate higher levels of cyberchondria and vice versa. In the present study, the internal consistencies were α=0.85 (compulsion), α=0.68 (distress), α=0.64 (excessiveness), α=0.66 (seeking reassurance), α=0.54 (mistrust of medical professional), and α=0.87 for the total scale.
The Short Health Anxiety Inventory (SHAI): The Short Health Anxiety Inventory (SHAI) [33] consists of 18 items assessing health anxiety. The scale was translated from English to Arabic and back-translated into English again by two independent bilingual psychologists’ expert in the field. Participants were asked to rate the frequency of each item on a Likert 4-point scale (from 0=never to 3=usually). Example items are: “I worry about my health”, “Resisting thoughts of illness is never a problem”, “If I have a bodily sensation or change, I wonder what it means” and “My family friends would say I worry enough about my health”. The internal consistency (Cronbach’s alpha) was α=0.81 for the total scale, α=0.71 for the subscale of health anxiety and feared likelihood of illness, and α=0.67 for the subscale of negative consequences of illness.
The Coronavirus Anxiety Syndrome Scale (CASS): The Coronavirus Anxiety Syndrome Scale (CAS) comprises 18 items that assesses COVID-19 anxiety; its items were written in Arabic to allow participants to fully understand the meaning of each item. Participants were asked to rate the frequency of each item on a 5-point scale (from 1=never to 5=almost every day). The total score ranges between 18 and 90, with a higher total score indicating higher COVID-19 anxiety syndrome levels. CASS comprises two subscales, namely, Sleep/eating disturbances (15 items, e.g., I had trouble falling asleep because of thinking about working during the coronavirus/ I lost appetite to eat when I was exposed to information about the coronavirus), and social distancing & home isolation problems (3 items, e.g., I feel depressed due to home isolation measures because of the coronavirus). The internal consistency (Cronbach’s alpha) was α =0.81 for the total scale, α=0.78 for the subscale of Sleep/eating disturbances and was α=0.74 for the subscale of social distancing & home isolation problems.
The Multidimensional Health Locus of Control – Form C (MHLC-C): The Multidimensional Health Locus of Control – Form C (MHLC-C) [34] was used to assess the participants’ locus of control. The original version of this instrument is written in English consisting of 18 items with a 6-point Likert response format ranging from strongly disagree=1 to strongly agree=6. The internal consistency (Cronbach’s alpha) was α=0.76 for the total scale, α=0.77 for the subscale of internal locus of control, α=0.68 for the subscale of chance and α=0.76 for the subscale of powerful others.
Statistical Analysis
Due to the lack of normal distribution of most of the study variables, Spearman's correlation coefficients were calculated. Repeated measures analyses of variance (rANOVA) were calculated for the course of the virus anxiety (the Greenhouse-Geisser adjustment was used to correct for violations of sphericity). In the mediation analyses, the total scores of the self- report measures were used (for health anxiety, the CSS, Health Locus of Control) and COVID-19 anxiety.
Results
Participants’ characteristics and anxiety related to COVID-19 anxiety
Table 2 shows participant characteristics with regard to questions specific to the COVID-19 pandemic and other self-report measures; SHAI, CSS, and HLoC. First, the characteristics of trait health anxiety (SHAI) and cyberchondria (CSS) were examined to describe the sample. Compared with a meta-analysis on the SHAI [35], the average score of the total SHAI in this study (M=41.58, SD=7.75) was slightly higher with a
small effect than the average score compared to an earlier study in the German general population [24]. With regards to gender variable, women reported higher scores than men in the subscale "compulsion"
(M men=20.72, SD=5.29; M women=19.87, SD=6.03)
with low to medium effect sizes (d=.073 – 0.250) and lower scores in the subscales "excessiveness" (M women=23.62, SD=6.26; M men=23.26, SD=6.65)
and "reassurance"
(M women=16.01, SD=4.66; Mmen=15.35, SD=5.10)
with low to medium effect sizes (d=0.68 – 0.382).
| |
M |
SD |
| COVID-19 pandemic |
|
|
| Sleep/Eating disturbance |
4.59 |
5.52 |
| Future anxiety |
14.5 |
7.56 |
| Infection anxiety |
3.95 |
2.06 |
| Social distancing and home isolation |
5.03 |
3.19 |
| Short Health anxiety inventory |
|
|
| Illness likelihood |
16.1 |
3.64 |
| Illness severity |
14.65 |
2.98 |
| Body vigilance |
10.83 |
2.74 |
| Cyberchondria Severity levels |
|
|
| Compulsion |
20.23 |
5.74 |
| Distress |
17.79 |
6.11 |
| Excessiveness |
23.46 |
6.43 |
| Reassurance |
15.73 |
4.86 |
| Mistrust of Medical Professional |
9.24 |
2.77 |
| Health Locus of Control |
|
|
| Internal control |
16.22 |
3.16 |
| Chance |
12.07 |
2.94 |
| Powerful Others |
17.76 |
3.31 |
Table 2. Participant characteristics with regard to questions specific to the COVID-19 pandemic and the self-report measures SHAI, CSSPandemic, and Health locus of control (N=573).
Table 3 presents descriptive statistics, reliability, and Pearson’s correlation coefficients for all measured variables. Cyberchondria was positively associated with health anxiety and COVID-19 symptoms, and was positively associated with health locus of control. On a related context, health
locus of control was also positively correlated with health anxiety, and positively with COID-19 anxiety. All variables tested in the mediation models were significantly interrelated though the correlation coefficients were very small.
| |
M |
SD |
1 |
2 |
3 |
4 |
| Cyberchondria |
86.46 |
18.24 |
1 |
|
|
|
| Health anxiety |
41.58 |
7.95 |
0.14** |
1 |
|
|
| Health locus of control |
46.05 |
6.53 |
0.29** |
0.60** |
1 |
|
| COVID-19 anxiety |
28.08 |
15.49 |
0.38** |
0.50** |
0.20** |
1 |
Table 3. Descriptive statistics and intercorrelations among all measured variables
Analysis of descriptive data also revealed that females had higher trait health anxiety compared with their male counterparts manifested by both SHAI scale and its subscales; SHAI(M women=41.90, SD=8.28; M men=41.15, SD=
7.74); illness likelihood (M women=16.18, SD=3.72; M men=15.99, SD=3.53);
illness severity
(M women=14.80, SD=3.70; M men=14.45, SD=2.84),
and body vigilance (M women=10.92, SD=2.86; M men=10.72, SD=2.54).
Females were also higher in their COVID-19
anxiety levels
(M women=28.54, SD=14.80; M men=27.45, SD=16.3
9). In terms of health locus of control, it was shown that individuals who think that their health issues are controlled through powerful others such as health professionals and health care providers (external locus of control) were more than the other two groups; internal control and chance control,
(M externalizers=17.86, SD=3.40; M internalizes=17.63, S D=3.18).
The findings revealed that cyberchondria severity was positively elated o health anxiety (r=0.14, p<0.07) and COVID-19 anxiety syndrome symptoms. Cyberchondria severity was also positively associated with health locus of control (r=0.29, p<.04). Health locus of control was also positively correlated with health anxiety (r=0.60, p<.02), and positively with COIVD-19 anxiety syndrome symptoms (r=0.53, p<.03).
To examine the mediation role of COVID-19 and health anxiety in the relationship between cyberchondria and health locus of control, simple mediation analysis was conducted with COVID-19 anxiety and health anxiety as potential mediators (see Figure 1). In the tested model COVID-19 anxiety was not related to health anxiety a1: = 0.13, SE=0.09, p<0.20, and COVID-19 anxiety
was not related to cyberchondria a2: =0.31, SE=0.03, p<0.001. On a related context, cyberchondria was related to health locus of control (b2: =0.14, SE=0.02, p<0.06). Based on the obtained model, COVID-19 anxiety can
predict the relationships among health anxiety, cyberchondria and health locus of control.
| Simple Model |
b |
SE |
95% CI |
P |
CSS COVID-19
anxiety (a2) |
0.6 |
0.03 |
-0.04 |
0.5 |
SHAI COVID-19
anxiety (a1) |
0.53 |
0.09 |
-0.38 |
0.16 |
| LoC CSS (b2) |
0.14 |
0.02 |
-0.058 |
0.69 |
Table 4. Mediation model
Covariates: demographic variables: nationality, gender, marital status, socio-economic level, time spent online and employment status. ci, confidence interval; css, cyberchondria severity scale; shai, sh ort health anxiety inventory; loc, locus of control.
It is clear that high levels of COVID-19 anxiety may cause feeling high levels of health anxiety that may consequently lead to enhanced internet overuse "cyberchondria" to search for medical information, people utilize internet to search medical information that help them to be knowledgeable about the infection features, precautionary procedures, as well as the valuable medications. For that reason, greater degrees of COVID-19 anxiety can mediate the relationship between health anxiety and excessive use of internet for searching medical information "cyberchondria".
Discussion
This study attempts to investigate the links between health anxiety, cyberchondria severity levels, and COVID-19 anxiety in the context of the current COVID-19 pandemic. It also investigated the health locus of control status; whether it is internal, chance, of powerful towards individuals’ health anxiety of COVID-19 pandemic. The associations between COVID-19 anxiety, health anxiety, and cyberchondria have also been assessed. In addition, the study aimed to assess whether COVID-19 mediate health anxiety and cyberchondria severity level. In particular, there are unfavorable effects of health anxiety exaggerated by COVID-19 pandemic which coincides with excessive information seeking activities and external locus of control (powerful others).
It is clear that females reported a slightly higher anxiety of COVID-19 infection, unlike studies which assess the gender differences in patients with COVID-19 that revealed that males are slightly higher than females in anxiety levels [36]. In line with recent studies on the COVID-19 pandemic [37,38], it was found that females reported higher levels of anxiety associated with the pandemic, a finding that is also consistent with the higher prevalence of anxiety disorders (and corresponding vulnerability factors) in females [24,39]. Another study coincides with this study revealed that females were found as risk factors for COVID-19 anxiety [24]. Higher levels of health anxiety lead to increased cyberchondria severity among study sample. However overall, the level of health anxiety can be described as relatively low compared to individuals with hypochondriasis [39]. It is possible that participants in the COVID- 19 pandemic may have reported higher scores in the SHAI. In a closely related study, cyberchondria accounted for 33% of health anxiety of the participants [35].
In addition, results revealed that COVID-19 anxiety level may lead to feeling high levels of health anxiety that may subsequently lead to increased internet use “cyberchondria”, individuals use internet to search medical information that that help them to be aware of the virus characteristics, precautionary procedures, and the useful drugs. Therefore, higher levels of COVID-19 anxiety can mediate the relationship between health anxiety and excessive use of internet for searching health information “cyberchondria”.
Conclusion
The current study is limited to investigating the relationship between COVID-19 anxiety, health anxiety, health locus of control in a sample of Arab individuals in Middle East and the Gulf States. Few studies assessed the actual relationship between cyberchondria and health anxiety during the current COVID-19 pandemic, especially that the combination of the two was associated with increased coronavirus anxiety. This study represents the first study to evaluate the difference between the study participants in terms of three variables; cyberchondria, health anxiety, and health locus of control in during COVID-19 pandemic. The study assessed the correlation between COVID-19 anxiety, health anxiety levels, and cyberchondria severity levels. Regarding potential buffering effects on anxiety, cyberchondria was positively associated with health anxiety and COVID-19 symptoms, it was positively associated with health locus of control. Health locus of control was also positively correlated with health anxiety, and positively with COVID-19 anxiety. It can be concluded that health anxiety serves as risk factor, whereas seeking medical information about the pandemic online and emotion regulation might represent buffering factors for COVID-19 anxiety during a virus pandemic.
One of the most important practical implications of the current study is to assess of the locus of control in health issues. It was revealed that the study participants view that health problems and therefore health anxiety can be alleviated/exaggerated through the actions of other people, i.e. external locus of control. This means that individuals usually depend mainly on health systems and health care providers to alleviate their health anxiety. The current study is significant due to the rarity of studies conducted in the Arab region that dealt with COVID-19 anxiety. After a thorough accurate investigation of literature, only two studies were detected. In addition, the study dealt with COVID-19 which adversely influenced the whole world in 2020, individuals living in Middle East and Gulf countries were not an exception. Also, a theoretical implication of the study is to conduct further studies and future research to assess the relationships between variables and to validate the model in other contexts.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- Tyrer P, Cooper S, Crawford M, Dupont S, Green J, & Murphy D, et al. Prevalence of health anxiety problems in medical clinics. Journal of psychosomatic research. 2011; 71: 392-4.
- Bandelow B, Michaelis S, & Wedekind, D. Treatment of anxiety disorders. Dialogues in clinical neuroscience. 2017; 19(2): 93–107.
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. 5th. American Psychiatric Association.
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders. 4th. Text Revision [Internet].
- Yates WR. Somatic Symptom Disorders Clinical Presentation. 2014.
- Pandey S, Parikh M, Brahmbhatt M, Vankar, GK. Clinical study of illness anxiety disorder in medical outpatients. Archives of Psychiatry and Psychotherapy. 2017; 4: 32–41.
- Hart J, Bjorgvinsson T. Health anxiety and hypochondriasis: Description and treatment issues highlighted through a case illustration. Bulletin of the Menninger Clinic. 2010; 74: 122–140.
- Starcevic V, Berle D. Cyberchondria: Towards a better understanding of excessive health-related internet use. Expert Review of Neurotherapeutics. 2013; 13(2): 205–213.
- Fox, S. The engaged E-population: People turn to the internet for health information when the stakes are high and the connections fast. 2008.
- Irving L, Klegar LK. Falling through the Net: Defining the Digital Divide. Washington, DC: US Department of Commerce. 1999.
- Lee K, Hoti K, Hughes JD, Emmerton L. Dr Google and the consumer: A qualitative study exploring the navigational needs and online health information-seeking behaviors of consumers with chronic health conditions. Journal of Medical Internet Research, 2014; 16: e262.
- Muse K, McManus F, Leung C, Meghreblian B, Williams J. Cyberchondriasis: Fact or fiction: A preliminary examination of the relationship between health anxiety and searching for health information on the internet. Journal of Anxiety Disorders. 2012; 26: 189–196.
- Powell JA. The doctor, the patient and the world-wide web: how the internet is changinghealthcare. Journal of the Royal Society ofMedicine. 2003; 96(2): 74-6.
- Uzun SU, Zencir M. Reliability and validity study of the Turkish version of cyberchondria severity scale. Current Psychology. 2018.
- Baumgartner SE, Hartmann T. The role of health anxiety in online health information search. Cyberpsychology, Behavior and Social Networking. 2011; 14(10): 613–618.
- Fergus, TA. The cyberchondria severity scale (CSS): An examination of structure and relations with health anxiety in a community sample. Journal of Anxiety Disorders. 2014; 28: 504–510.
- Turkiewicz KL. The impact of cyberchondria on doctor-patient communication. Unpublished doctoral dissertation. The University of Wisconsin, Milwaukee. 2012.
- Mackenzie JS, David WS. COVID-19: A novel zoonotic disease caused by a coronavirus from China: what we know and what we don't.” Microbiology Australia. 2020,
- Eysenbach G. Towards quality management of medical information on the internet: evaluation, labelling, and filtering of information. British Medical Journal. 1998; 317: 1496-1502.
- Jadad AR, Gagliardi A. Rating health information on the Internet: Navigating to knowledge or to Babel. Journal of the American Medical Association. 1998; 279(8): 611-614
- Eysenbach G, Kohler C. How do consumers search for and appraise health information on the worldwide Web? Qualitative studies using focus groups, usability test, and in-depth interviews. British Medical Journal. 2002; 324: 573-577.
- Wallston KA, Wallston BS, DeVellis R. Development of the Multidimensional Health Locus of Control (MHLC) Scales. Heath EducMonogr. 1978; 6(2):160-70. 10.
- Wallston K., Stein MJ, Smith CA. Form C of the MHLC Scale: A condition-specific measure of locus of control. Journal of Personality Assessment. 1995; 63(3): 534-53.
- Özdin S, Özdin SB. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. International Journal of Social Psychiatry. 2020: 1–8.
- Liu PL. COVID-19 information seeking on digital media and preventive behaviors: The mediation role of worry. Cyberpsychology, Behavior, and Social Networking. 2020.
- Ebrahim AH, Saif ZQ, Buheji M, AlBasri N, Al-Husaini FA, Jahrami H. COVID-19 Information-Seeking Behavior and Anxiety Symptoms among Parents. OSP Journal of Health Care and Medicine. 2020; 1(1): 1-9.
- Ahmad AR, Murad HR. The Impact of Social Media on Panic during the COVID-19 Pandemic in Iraqi Kurdistan: Online Questionnaire Study. Journal of Medical Internet Research. 2020; 22(5): e19556.
- Naviaux AF, Janne P, Gourdin M. Response- Ability facing Covid-19: A matter of psyche, behavior and civism. Journal of Clinical Immunology & Immunotherapy Category.
- Pourhoseinzadeh M. The Relationship between Health Locus of Control and Health Behaviors in Emergency Medicine Personnel. International journal of community-based nursing and midwifery. 2017; 5(4): 397-407.
- Ma Y, Wang D, Yuan, M. et al. (2019). The mediating effect of health anxiety in the relationship between functional somatic symptoms and illness behavior in Chinese inpatients with depression. BMC Psychiatry. 2019; 19: 260.
- Asmundson GJG, Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision- makers, health authorities, and health care professionals need to know. Journal of Anxiety Disorders. 2020; 71.
- McElroy E, Shevlin M. The development and initial validation of the Cyberchondria Severity Scale (CSS). Journal of Anxiety Disorders. 2014; 28: 259–265.
- Rimes K, Clark MD. The health anxiety inventory: Development and validation of Scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine. 2002; 32: 843-853.
- Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020; 287
- Alberts NM, Hadjistavropoulos HD, Jones SL. The Short Health Anxiety Inventory: A systematic review and meta-analysis. Journal of Anxiety Disorders. 2013; 27: 68–78
- Geertzen JH, Van Wilgen CP, Schrier E, Dijkstra PU. Chronic pain in Rehabilitation Medicine. Disability Rehabilitation. 2006; 28(6): 363-7.
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian Journal of Psychiatry. 2020; 51.
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, XuY. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry, 2020: 33(2)
- Remes O, Brayne C, van der Linde R, Lafortune L. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain and Behaviour. 2016: 6(7)