COLLATERAL CIRCULATION CHARACTERISTIC BASED ON CONE BEAM COMPUTED TOMOGRAPHY (CBCT) IMAGES IN HYPERACUTE STROKE
1Department of Engineering and Technology, Multimedia University, Melaka, Malaysia
2Department of Radiology, Hospital Pengajar UPM, FPSK, Universiti Putra Malaysia, Selangor, Malaysia
3Department of Electrical Engineering, Universiti Teknikal Malaysia Melaka, Malaysia
4Department of Electrical & Electronic Engineering Technology, Universiti Teknikal Malaysia Melaka, Malaysia
5Department of Psychiatry, Faculty of Medicine, Universiti Teknologi MARA (UiTM), 47000 Sg. Buloh, Selangor, Malaysia
*Corresponding Author:
Nur Hasanah ALI, Department of Engineering and Technology, Multimedia University,
Melaka,
Malaysia,
Email: hasanah.ali@mmu.edu.my
Received: 26-Sep-2022, Manuscript No. AJOPY-22-77940;
Editor assigned: 27-Sep-2022, Pre QC No. AJOPY-22-77940 (PQ);
Reviewed: 14-Oct-2022, QC No. AJOPY-22-77940;
Revised: 21-Oct-2022, Manuscript No. AJOPY-22-77940 (R);
Published:
28-Oct-2022, DOI: 10.54615/2231-7805.47307
Abstract
Good collateral circulation flow is a promising outcome for ischemic stroke patients. Collateral circulation is the vessels that flow in parallel to each other, perfusing the same target tissue. Different patients are shown to have different statuses of collateral. Good collateral circulation is expected to give significantly better clinical outcomes for stroke patients including acute stroke patients who underwent thrombectomy. Modern multimodal imaging techniques have encouraged neuroradiology to assess collateral flow. This paper presents the basic overview of CBCT technology and compares the usefulness of Cone Beam Computed Tomography (CBCT), Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) based on working principles, performance, cost and applications. In addition, the overview of collateral circulation and its characteristics will be discussed. In assessing collateral circulation, improvement of acquisition techniques and algorithm CBCT provides fast delineation of detail vasculature and improves spatial resolution. It is a three-dimensional (3D) imaging modality to investigate collateral flow. For ischemic stroke patients with clinical symptoms, CBCT improves the image quality for the assessment of collateral circulation in the brain. Precise evaluation of collateral circulation from the images will support the decision-making for suitable acute stroke treatment, benefiting both the patient and doctor. ASEAN Journal of Psychiatry, Vol. 23(10) October, 2022; 1-13.
Keywords
Stroke; Collateral circulation; CBCT; Neuroimaging.
Introduction
Stroke is one of the leading causes of death in Malaysia. In 2019, stroke deaths accounted for 8% of the total 109,164 deaths in Malaysia. Most strokes occur due to an anticipated obstruction of blood flow to multiple areas of the brain and require revascularization within 6 hours [1,2]. A lack of nutrients and oxygen to the cells in these areas of the brain leads to cell death and some other serious problems such as blood vessel ruptures. Women have a higher risk of developing a stroke-related disease than men, namely 6 in 10 people. There are inherent risks associated with thrombectomy, but only for patients with some characteristics. For example, a small infarction with a large penumbra, and excellent collateral circulation, should undergo such a procedure.
In this paper, the concept of collateral circulation classification using CBCT is discussed. In the brain, collateral circulation is understood as a network of artery-to-artery anastomoses that can provide nutrient perfusion when a region has suffered a reduction in blood flow [3]. Collateral circulation is essential to maintain blood flow to ischemic sites in various stages of ischemic stroke including the hyperacute phase [4]. Good collateral circulation has been shown to result in a favorable functional outcome and reduced risk of recurrence in those undergoing endovascular treatment or medical management [5]. Different imaging scores can be used to quantify collateral cerebral blood flow [6]. How collateral circulation helps patients with ischemic stroke is actively studied and evaluated. Since the collateral circulation is critical for assessing the presence and volume of the penumbra, which are critical factors in the severity and time course of ischemic stroke, the status of the collateral circulation is critical.
A cerebral collateral image provides rich details regarding the flow of blood to different parts of the brain; the characteristics of this blood flow, as opposed to an arterial lesion, determine whether the underlying brain parenchyma survives. For an image of cerebral collateral, the assessment of collateral-dependent blood flow is one of the popular techniques [7,8], and it is observed better by using CBCT. CBCT gives a higher quality of spatial resolution as compared to conventional CT which gives better contrast resolution. Depending on how much retrograde filling is needed, the sub-branches of the cerebral artery trees will be viewable, and the status of collateral will also be determined to some static extent [9].
Nowadays, CBCT is widely accepted as the evaluation requirement for stroke disease, due to its familiarity, better spatial resolution, and wide availability to doctors [10]. However, it is still not a standard procedure as it is time-consuming and difficult to perform CBCT. In addition, unavoidable risks such as allergic and radiation exposure are major shortcomings of this approach [11]. Since collateral circulation recruitment is essential to influence stroke outcomes, accurate and robust collateral circulation metrics are required. In addition, with digitalization taking over the health industry, machine learning can also help to fasten the diagnosis through segmentation and classification processes [12].
Cone Beam Computed Tomography (CBCT)
Cone beam computed tomography, is an advanced imaging technology that provides accurate three- dimensional (3D) images of hard tissue, soft tissue, and bone [13]. As a result of its advantages over conventional CT, CBCT is increasingly used in acute strokes and neurovascular image-guided procedures including strokes and nerve damage [14,15]. The data must be acquired using a CT-based algorithm to create volumetric data that can be seen in various possible planes in addition to the three standard planes of sagittal, axial, and coronal. The scan is relatively fast ranging from 4 to 20 seconds acquisition time, utilizing the latest technology. The region of interest is visualized in 3 dimensions, however, the resolution is insufficient to identify the associated anatomy in 2 dimensions [16].
Some devices are motorized on numerous axes for Advance CBCT applications to allow the source- detector of monocentric. To enhance and improve the Field Of View (FOV) in three-dimension image reconstructions, the views of specialized radiography and fluoroscopic must be repositioned rapidly. Several systems, including some Cone Beam Computed Tomography mammography systems and C-arm systems, can perform complicated source-detector trajectories [17]. The added flexibility given by these systems allows for more generic imaging beyond the usual circular and helical source-detector paths. These variable angles have mostly been employed to overcome the FOV and sampling concerns in interventional CBCT. Noncircular trajectories, for an instance, have been employed to give expanded axial and elliptical types of FOV as well as to increase three-dimensional sampling and data collection to prevent cone-beam artifacts caused by standard circular cone-beam.
The quality of a CBCT picture might vary greatly depending on the patient's anatomical position, size, and the occurrence of interventional devices inside the field of view. Although a single scan for a single patient, data quality can be changed obviously, the magnitude variance order in noise for various parameters will also be manipulated. This research aims to create a novel imaging process in which CBCT scans are guided by the anatomy of the patient, selecting projections that maximize data quality for a given bio-medical imaging job. In general, trajectory design necessitates some understanding of patient anatomy.
Such data is frequently accessible in interventional imaging, although it is rarely used directly by the imaging apparatus [18]. In this research, CBCT images are obtained from Hospital Pengajar Universiti Putra Malaysia(HPUPM) using an angiography system machine. Neurointerventionist (Philips Allura; Biplane FD 20/15) who performs CBCT scans is required to ensure that the output image is reviewed and reported [19]. Figure 1 shows the CBCT image that has been used in this research to identify the collateral circulation class.
Table 1 shows the comparison between CBCT, CT and MRI. CT-based MR image construction is one of the techniques that researchers need to discuss as it is difficult to construct image quality domains based on low-level image domains when producing an MR image immediately from a CT imaging using a linear model [20]. CT and MRI stroke protocols are routinely used to make treatment recommendations in the ischemia period, providing reperfusion of ischemic penumbra [21]. There is a way to map a set of loss terms to a number that intuitively represents the cost of a particular network state as defined by its objective function [22]. During medical imaging, synthetic images need to not only be realistic, i.e., that human experts cannot differentiate them from genuine images, but also have some similarity to reference images.
| |
CBCT |
CT |
MRI |
| Working principle |
Uses of X-ray computed tomography technology with divergent, forming a 360-degree rotation (Lata et al., 2018). |
Uses multiple X-rays with different angles (Walter et al., 2020). |
Uses of magnetic fields with different RF pulses (Jin et al., 2019). |
| Scanning time |
Lower scanning time (Lei et al., 2020) |
Moderate scanning time (Lei et al., 2020) |
Longest scanning time (Lei et al., 2020) |
| Level of radiation exposure |
Lower level of radiation exposure (Kabaliuk et al., 2017) |
Minimum level of radiation exposure (Kabaliuk et al., 2017) |
No radiation exposure (Kabaliuk et al., 2017) |
| Imaging movement |
Largest imaging movement (Kabaliuk et al., 2017) |
Slight imaging movement (Kabaliuk et al., 2017) |
No imaging movement (Kabaliuk et al., 2017) |
| Cost |
Lower Cost (Jeon et al., 2020) |
Moderate cost (Jeon et al., 2020) |
Most expensive (Jeon et al., 2020) |
| Image quality/accuracy |
Lowest image quality and less accuracy (Jeon et al., 2020) |
Moderate image quality and accuracy (Jeon et al., 2020) |
Highest image quality and most accuracy (Jeon et al., 2020) |
| Application |
Provide a medical image in the dentistry field such as oral surgery, endodontics, orthodontics, and so on (Jin et al., 2019) |
Provides an area of a medical image such as head trauma, bone fractures, or internal organs (Jin et al., 2019) |
Provides detailed medical images such as soft tissue diagnosis and ligaments (Jin et al., 2019) |
| Drawbacks |
Poor contrast resolution (Lei et al., 2020) |
Harmful to humans (Lei et al., 2020) |
Loud noises produced by MRI scanners will lead to hearing problems (Jin et al., 2019) |
| Radiation effect |
Low radiation (Shokri et al., 2018) |
High radiation (Meulepas et al., 2019) |
No radiation (Indra J Das et al., 2018) |
Table 1. Comparison Table of CBCT, CT and MRI.
Generally, CT is the most commonly used modality for stroke imaging followed closely by MRI. Computed tomography is also more easily accessible than MRI. However, MRI is more accurate in depicting acute stroke [23], but perceived high loss and complexity of the sequences, making MRI not the preferred choice for neuroimaging in acute stroke. However, there is increasing adoption of the MRI-first policy in acute stroke [24]. As compared to MSU and low-field MR scanning, contemporary fixed MRI scanners provide a significant number of advantages. When combined with individualized patient transportation and assessing strategy, these scanners provide more diagnostics and temporal accessibility [25,26].
Collateral Circulation
Overview
Collaterals are defined as vessels that run parallel to each other transporting blood to the same target tissue. Collateral circulation acts as a vascular supplementary system. It also plays a significant role in the prevention of cerebral ischemia after the primary vascular pathways have been partially blocked [27]. Collateral circulation has long-term consequences in management, especially concerning cerebral endovascular therapy and thrombolytic therapy.
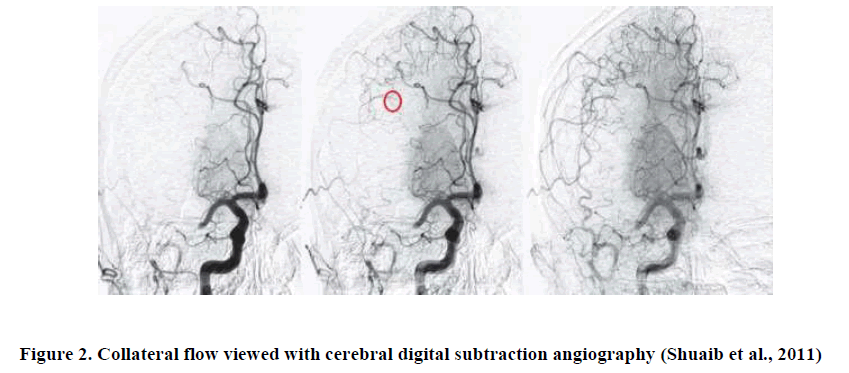
It is regarded as a secondary network of extremely changeable vascular channels and beneficial in the condition of inadequate arterial supply. Besides the arterial collaterals, there are also venous collaterals. Their function differs, however they aid in the enhancement of venous drainage in venous congestion [28]. Several pharmacological interventions are employed to alter the assets pledged as collateral; these could act as an alternative to invasive intracerebral surgeries [29,30]. Figure 2 shows the collateral circulation in the human brain.
Endovascular treatment for acute ischemic stroke could be enhanced using good collateral circulation and reduced risk of hemorrhagic transformation [31]. Understanding of collaterals and the strategy to promote new collateral blood flow is necessary during brain ischemia to increase collateral blood flow, a crucial aspect of treating ischemic stroke is extending the therapeutic time window following ischemia [32]. When pressure gradients arise, pre-existing communication routes are used. Normal ICA perfusion is occasionally maintained in the context of common carotid artery (CCA) obstruction by retrograde blood flow within the External Carotid Artery (ECA). Abnormal blood flow inside collateral channels is a common observation in both acute and chronic strokes. Every hemodynamically important extracranial flow blockage results in compensatory intracranial flow changes [33].
Collateral Circulation Characteristics
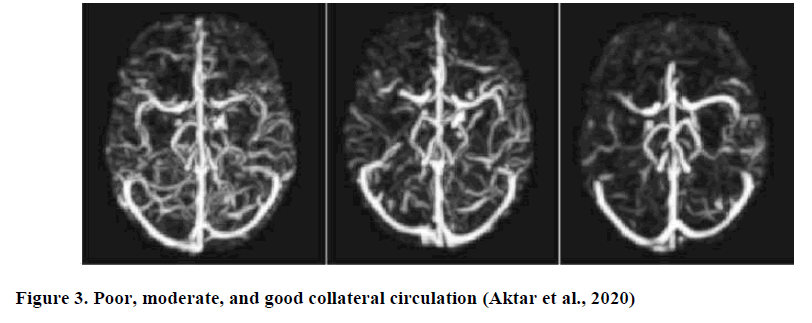
Previous analysis of collateral circulation was classified into three classes: good, moderate and poor. These classes are referred to based on the collateral supply in the blocked MCA territory according to ASPECTS [34]. According to Jiahang Su et al., patients having good collateral scores will most likely have better clinical outcomes used the ASPECTS score as ground truth in the experiments and also based on the validation by two radiologists. Figure 3 shows the class of collateral circulation which is interpreted as 100% score of good collaterals, between 50% and 100% of intermediate collaterals and <50% of poor collaterals [35-40]( Figure 3).
Each class of collateral circulation has its characteristics. Table 2 shows the comparison of poor, moderate, and good collateral circulation [41,42].
| |
Poor Collateral Circulation |
Moderate Collateral Circulation |
Good Collateral Circulation |
| Evaluation using the Miteff collateral method |
Only superficial MCA is reconstructed distal to the occlusion (Liu et al., 2018) |
Some of the MCA branches are reconstructed distal to the occlusion (Liu et al., 2018) |
Most of the MCA branches are reconstructed distal to the occlusion (Liu et al., 2018) |
| Number of collateral paths |
Least number of collateral paths (Kolateralne et al., 2018; Wang et al., 2020) |
Moderate number of collateral paths (Kolateralne et al., 2018; Wang et al., 2020) |
Most number of collateral paths (Kolateralne et al., 2018; Wang et al., 2020) |
| Collateral Score |
Ischemic collaterals slowly spread to the periphery of the ischemic site with some defects persisting (Kolateralne et al., 2018; Wang et al.,2020) |
Slow collaterals but the angiographic blood flow of the ischemic bed is completed (Kolateralne et al., 2018; Wang et al., 2020) |
Retrograde perfusion provides comprehensive and efficient collateral blood flow to the vascular bed across the ischemic zone (Kolateralne et al., 2018; Wang et al., 2020) |
| Overall performance |
A portion of the distal vessel segment was reconstituted with |
An occluded vessel was reconstructed with collaterals located at the |
Two segments of vessels were reconstituted distal to the occluded vessel |
| |
collaterals (Boers et al., 2018; Fujita et al., 2019; Raychev et al., 2020; Renú et al., 2019; Vagal et al., 2018) |
distal end of the segment (Boers et al., 2018; Fujita et al., 2019; Raychev et al., 2020; Renú et al., 2019; Vagal et al., 2018) |
using collaterals (Boers et al., 2018; Fujita et al., 2019; Raychev et al., 2020; Renú et al., 2019; Vagal et al., 2018) |
Table 2. Comparison of poor, moderate, and good collateral circulation.
Enhancement of collateral circulation is considered a crucial strategy for better clinical outcomes. Collateral status may be negatively impacted by the optimization of factors, including medications that inhibit physiological augmentation of blood pressure, systemic sickness, and cerebral vascular status [43]. Induced hypertension, lying flat with the head in that position, volume expansion, external counterpulsation, a partial aortic obstruction that directs splanchnic blood flow to the upper body and brain, and stimulation of the sphenopalatine ganglion are all collateral enhancing techniques for hemodynamic manipulations [44] as well as emergent bypass surgery [45] could help acute ischemic stroke patient.
Conclusion
Collateral circulation using CBCT images comprises strong anastomotic cerebral vessels for better reperfusion of ischemic tissue. The good collateral vessels can maintain an adequate blood flow towards the ischemic penumbra that making the reperfusion more efficient. The recent achievement of clinical results showed that the beneficial influence of the initial assessment of collateral adequacy is very important to have better clinical outcomes. Clinical trials using more advanced methods are predicted to provide clinical interpretation for more reliable use of collaterals for potential clinical impact [45-50].
Acknowledgement
The authors would like to thanks the Universiti Teknikal Malaysia Melaka (UTeM), Faculty of Electrical and Electronic Engineering Technology (FTKEE) and Faculty of Electrical Engineering (FKE), Advance Digital Signal Processing (ADSP) Lab, and Ministry of Higher Education (MOHE), Malaysia that supported this research project.
References
- Aziz AA, Izhar LI, Asirvadam VS, Tang TB, Ajam A, et al., Detection of Collaterals from Cone-Beam CT Images in Stroke. Sensors 2021; 21(23):80-99.
[Crossref][Google Scholar][PubMed]
- Aktar M, Tampieri D, Rivaz H, Oertel MK, Xiao Y Automatic collateral circulation scoring in ischemic stroke using 4D CT angiography with low-rank and sparse matrix decomposition. Int J Comput Assist Radiol Surg 2020; 15(9); 1501-1511.
[Crossref][Google Scholar][PubMed]
- Albers GW, Marks MP, Kemp Christensen S, Tsai JP, et al., Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N Engl J Med, 378(8), 708-718.
[Crossref][Google Scholar][PubMed]
- Ali NH, Abdullah AR, Saad NM, Muda AS, Sutikno T, et al., Brain stroke computedtomography images analysis using image processing: A Review. IAES International Journal of Artificial Intelligence (IJ-AI) 2021; 10(4): 1048.
[Crossref][Google Scholar]
- Barthels D, Das H. Current advances in ischemic stroke research and therapies. Biochim Biophys Acta Mol Basis Dis 2020; 1866(4): 165260.
[Crossref][Google Scholar][PubMed]
- Aziz MA, Jalil SZA, Rahaman SASA, Abdullah H, Ismail SH et al., Development of Speech Therapy Mobile Application for Aphasia Patients. 2021 IEEE 11th International Conference on System Engineering and Technology (ICSET) 2021; pp: 130-133.
[Crossref][Google Scholar]
- Bhat SS, Fernandes TT, Poojar P, Ferreira MDS, Rao PC, et al., Low-Field MRI of Stroke: Challenges and Opportunities. J Magn Reson Imaging 2021, 54(2): 372- 390.
[Crossref][Google Scholar][PubMed]
- Maier IL, Scalzo F, Leyhe JR, Schregel K, Behme D, et al.,Validation of collateral scoring on flat-detector multiphase CT angiography in patients with acute ischemic stroke. PLoS ONE 2018; 13(8): 1-9.
[Crossref][Google Scholar][PubMed]
- Dief S, Keenan AV, Amintavakoli N, McGowan R. A systematic review on incidental findings in cone beam computed tomography (CBCT) scans. Dentomaxillofacial Radiology 2019; 48(7): 20180396.
[Crossref][Google Scholar][PubMed]
- Drage N. Cone Beam Computed Tomography (CBCT) in General Dental Practice. Prim Dent J 2018; 7(1): 26-30.
[Crossref][Google Scholar][PubMed]
- Fujita K, Tanaka K, Yamagami H, Ide T, Ishiyama H, et al., Detrimental Effect of Chronic Hypertension on Leptomeningeal Collateral Flow in Acute Ischemic Stroke. Stroke 2019, 50(7): 1751-1757.
[Crossref][Google Scholar][PubMed]
- Grunwald IQ, Kulikovski J, Reith W, Gerry S, Namias R, et al., Collateral Automation for Triage in Stroke: Evaluating Automated Scoring of Collaterals in Acute Stroke on Computed Tomography Scans. Cerebrovasc Dis 2019; 47(5-6): 217-222.
[Crossref][Google Scholar][PubMed]
- Gyojun H, Wan OC, Seung BJ, Kyu JC, O- Ki K, et al., Superficial Temporal Artery to Middle Cerebral Artery Bypass in Acute Ischemic Stroke and Stroke in Progress. Neurosurgery 2011; 68(3): 723-729.
[Crossref][Google Scholar]
- Das IJ, McGee KP, Tyagi N, Wang H. Role and Future of MRI in Radiation Oncology. Br J Radiol 2019; 92: 1094.
[Crossref][Google Scholar][PubMed]
- Jeon KJ, Lee C, Choi YJ, Han SS. Comparison of the Usefulness of CBCT and MRI in TMD Patients According To Clinical Symptoms and Age. Appl Sci 2020; 10(10): 3599.
[Crossref][Google Scholar]
- Jin CB, Kim H, Liu M, Han IH, Lee JI, et al., DC2Anet: Generating Lumbar Spine MR Images from CT Scan Data Based on Semi-Supervised Learning. Appl Sci 2019; 9(12): 2521.
[Crossref][Google Scholar]
- Kabaliuk N, Nejati A, Loch C, Schwass D, Cater JE, et al., Strategies for Segmenting the Upper Airway in Cone-Beam Computed Tomography (CBCT) Data. Open Journal of Medical Imaging, 2017; 07(04): 196-219.
[Crossref][Google Scholar]
- Kaps M. Extracranial and intracranial collateral pathways. Manual of Neurosonology 2016; 165–168.
[Crossref][Google Scholar]
- Kolateralne Z, Kod C, Ishemijskog A, Udara M. The Significance of collateral circulation in acute ischemic stroke. Med Pregl 2018; 46: 3302-3309.
[Google Scholar]
- Lata S, Mohanty SK, Vinay S, Das AC, Das S, et al., “Is Cone Beam Computed Tomography (CBCT) a Potential Imaging Tool in ENT Practice?: A Cross-Sectional Survey Among ENT Surgeons in the State of Odisha, India. Indian J Otolaryngol Head Nec 2018; 70(1): 130-136.
[Crossref][Google Scholar][PubMed]
- Lechuga L, Weidlich GA. Cone Beam CT vs. Fan Beam CT: A Comparison of Image Quality and Dose Delivered Between Two Differing CT Imaging Modalities. Cureus 2016; 8(9): e778.
[Crossref][Google Scholar][PubMed]
- Lei Y, Wang T, Tian S, Dong X, Jani AB, et al., Male pelvic multi-organ segmentation aided by CBCT-based synthetic MRI. Physics in Medicine and Biology 2020; 65(3).
[Crossref][Google Scholar][PubMed]
- Liu L, Ding J, Leng X, Pu Y, Huang LA, et al., Guidelines for evaluation and management of cerebral collateral circulation in ischaemic stroke 2017. Stroke Vasc Neurol 2018; 3(3): 117-130.
[Crossref][Google Scholar][PubMed]
- https://emedicine.medscape.com/article/19 16852-treatment
- Malhotra K, Liebeskind DS. Collaterals in ischemic stroke. Brain Hemorrhages 2020; 1(1): 6-12.
[Crossref][Google Scholar][PubMed]
- Malhotra K, Safouris A, Goyal N, Arthur A, Liebeskind DS, et al., Association of statin pretreatment with collateral circulation and final infarct volume in acute ischemic stroke patients: A meta-analysis. Atherosclerosis 2019; 282(11): 75-79.
[Crossref][Google Scholar][PubMed]
- Meulepas JM, Ronckers CM, Nievelstein RAJ, Gradowska P, Hauptmann M, et al., Radiation exposure from pediatric CT scans and subsequent cancer risk in the Netherlands. J Natl Cancer 2019; 111(3): 256-263.
[Crossref][Google Scholar] [PubMed]
- Muda AS, Kamis MFAK, Mohd Yaakob MN, Abdul Rahim E, Mahmood MK, et al., Putra acute stroke protocol. Journal of Cardiovascular 2021; 3(4): 12–14.
[Crossref][Google Scholar]
- Olavarría VV, Arima H, Anderson CS, Brunser AM, Muñoz-Venturelli P, et al., Head position and cerebral blood flow velocity in acute ischemic stroke: A systematic review and meta-analysis. Cerebrovascular Diseases 2014; 37(6): 401–408.
[Crossref][Google Scholar] [PubMed]
- Patel S, Brown J, Pimentel T, Kelly RD, Abella F, et al., Cone beam computed tomography in Endodontics – a review of the literature. Int Endod J 2019; 52(8): 1138–1152.
[Crossref][Google Scholar] [PubMed]
- Paul S, Candelario-Jalil E. Emerging neuroprotective strategies for the treatment of ischemic stroke: An overview of clinical and preclinical studies. In Experimental Neurology 2021; 335: 113-518.
[Crossref][Google Scholar] [PubMed]
- Piedade GS, Schirmer CM, Goren O, Zhang H, Aghajanian A, et al., Cerebral Collateral Circulation: A Review in the Context of Ischemic Stroke and Mechanical Thrombectomy. World Neurosurgery 2019; 122: 33–42.
[Crossref][Google Scholar] [PubMed]
- Potter CA, Vagal AS, Goyal M, Nunez DB, Leslie-Mazwi TM, et al., Ct for treatment selection in acute ischemic stroke: A code stroke primer. Radiographics 2019; 39(6): 1717–1738.
[Crossref][Google Scholar] [PubMed]
- Detection of Collaterals
- Raychev R, Liebeskind DS, Yoo AJ, Rasmussen M, Arnaudov D, et al., Physiologic predictors of collateral circulation and infarct growth during anesthesia – Detailed analyses of the GOLIATH trial. J Cereb Blood Flow Metab 2020; 40(6): 1203–1212.
[Crossref][Google Scholar] [PubMed]
- Renú A, Laredo C, Montejo C, Zhao Y, Rudilosso S, et al., Greater infarct growth limiting effect of mechanical thrombectomy in stroke patients with poor collaterals. J Neurointerv Surg 2019; 11(10): 989–993.
[Crossref][Google Scholar] [PubMed]
- Santos EMM, d’Esterre CD, Treurniet KM, Niessen WJ, Najm M, et al., Added value of multiphase CTA imaging for thrombus perviousness assessment. Neuroradiology 2018; 60(1): 71–79.
[Crossref][Google Scholar] [PubMed]
- Schlotman AA, Donahue MJ, Kassim AA, Lee CA, Waddle SL, et al., Intracranial and Extracranial Vascular Stenosis as Risk Factors for Stroke in Sickle Cell Disease. Pediatric Neurology 2021; 114: 29–34.
[Crossref][Google Scholar] [PubMed]
- Shokri A, Eskandarloo A, Norouzi M, Poorolajal J, Majidi G, et al., Diagnostic accuracy of cone-beam computed tomography scans with high- and low- resolution modes for the detection of root perforations. Imaging Sci Dent 2018; 48(1): 11–19.
[Crossref][Google Scholar] [PubMed]
- Shuaib A, Butcher K, Mohammad AA, Saqqur M, Liebeskind DS. Collateral blood vessels in acute ischaemic stroke: A potential therapeutic target. The Lancet Neurology 2011; 10(10): 909–921.
[Crossref][Google Scholar] [PubMed]
- Stayman JW, Capostagno S, Gang GJ, Siewerdsen JH. Task-driven source– detector trajectories in cone-beam computed tomography: I. Theory and methods. J Med Imaging 2019; 6(2): 1.
[Crossref][Google Scholar] [PubMed]
- Su J, Wolff L, Zwam WV, Majoie C, Niessen WJ, Walsum TV. Automatic Collateral Scoring From 3D CTA Images. IEEE Transactions on Medical Imaging 2020; 39(6): 2190–2200.
[Crossref][Google Scholar] [PubMed]
- Tong LS, Zhen G, X cheng, Tang J, Zhang JH, Lou M. et al., Cerebral venous collaterals: A new fort for fighting ischemic stroke. Progress in Neurobiology 2018; 163: 172–193.
[Crossref][Google Scholar] [PubMed]
- Vagal A, Aviv R, Sucharew H, Reddy M, Hou Q, Michel P, et al., (2018) Collateral clock is more important than time clock for tissue fate a natural history study of acute ischemic strokes 49(9): 2102–2107.
[Crossref][Google Scholar] [PubMed]
- Vasquez HE, Murlimanju BV, Shrivastava A, Durango-Espinosa YA, Joaquim AF, e al., Intracranial collateral circulation and its role in neurovascular pathology. Egypt J Neurosurg 2021; 36(1): 0–4.
[Crossref][Google Scholar]
- Verdolotti, T, Pilato F, Cottonaro S, Monelli E, Giordano C, et al., Colorviz, a new and rapid tool for assessing collateral circulation during stroke. Brain Sciences 2020; 10(11): 1–8.
[Crossref][Google Scholar] [PubMed]
- Vymazal J, Rulseh AM, Keller J, Janouskova L. Comparison of CT and MR imaging in ischemic stroke. Insights into Imaging 2012; 3(6): 619–627.
[Crossref][Google Scholar] [PubMed]
- Walter C, Schmidt JC, Rinne CA, Mendes S, Dula K, et al., Cone beam computed tomography (CBCT) for diagnosis and treatment planning in periodontology: SYstematic review update. Clin. Oral Investig 2020; 24(9): 2943–2958.
[Crossref][Google Scholar] [PubMed]
- Wang Z, Ding J, Bai C, Ding Y, Ji X, Meng R. Clinical Classification and Collateral Circulation in Chronic Cerebrospinal Venous Insufficiency. Frontiers in Neurology 2020; 11(10): 1–9.
[Crossref][Google Scholar] [PubMed]
- Yang F, Zhang D, Zhang H, Huang K. Cupping artifacts correction for polychromatic X-ray cone-beam computed tomography based on projection compensation and hardening behavior. Biomed Signal Process Control 2020; 57: 101-823.
[Crossref][Google Scholar]
Citation: Collateral Circulation Characteristic Based on Cone Beam Computed Tomography (Cbct) Images in
Hyperacute Stroke ASEAN Journal of Psychiatry, Vol. 24(4) April, 2023; 1-13.