Introduction
Hospital Mesra Bukit Padang is one of four
mental institutions under the Malaysian Ministry
of Health (MMH). Each covering multiple states,
the facilities are tasked to treat the mentally ill,
both civil and forensic. It is common to have
long stay chronic wards in mental institutions
and aside from the one reserved for Criminal
Procedure Code (CPC) section 348 (patients
ordered by the civil court to be held in ward),
there are several chronic wards in HMBP (male
and female) [1].
Throughout the years, it was found that the
number of psychiatric patients is increasing,
along with inpatient admission as well. After
completing their acute treatment in HMBP, the
doctors found difficulties to discharge these
patients back to their home [2]. Most of them,
with their mental health stabilized, found to have
social issues which the clinicians and allied
health units have difficulty resolving. There were
not many options available during discussions:
To continue trying to contact and negotiate with
the families or continue keeping these patients by transferring them to chronic wards. As
establishing our center to be a center of
excellence is our vision and hoping to improve
the mental health services, a solution must be
found in reducing mental institutionalization in
Sabah.
Materials and Methods
Mental institutions are tasked to treat the
mentally ill and to house those who are deemed
unable to return to the normal society. After
United Nation and WHO declare the policies of
deinstitutionalization (WHO: The World Health
Report 2001), multiple studies have mentioned
about the rationale of the implementation. The
main struggle has always been the economic
burden of institutionalization [3].
With the prevalence of mental illness increases,
without the community’s support, hospital Mesra
have faced issues of full occupancy, which leads
to the same financial difficulties as mentioned
earlier, staggering the quality of care provided to
the patients [4].
Knapp, et al. has reported in 2011 that the effort
of de-institutionalization must be done right with
the cooperation of multiple agencies. By having
a well-developed system in the community
setting, the overall cost of treatment can be
vastly reduced. Otherwise, it would just be the
same as diverting the cost to other organizations.
In this study we hope to address the issue of high
Bed Occupancy Rate (BOR) in HMBP. We
gather data of the common reasons for patient
admission to chronic wards and find which ones
are associated to patient having difficulty to be
discharged home. Among those reasons, we
would also be looking at the illness perspective,
whereby does the severity of their illness play a
role? With that information, we hope to develop
a solution to the issue [5].
To assess the severity of a psychiatric illness, we
chose the Brief Psychiatry Rating Scale (BPRS)
version 4.0 as it is a validated widely used
clinician rated assessment tool with good validity
and reliability.
The BPRS is a widely used measurement
instrument to assess the changes in severity in
psychopathology in a wide variety of severe
psychiatric disorders, such as schizophrenia,
depression and bipolar disorders which are found
to be common diagnoses in the chronic wards.
The BPRS version 4.0 includes an expanded twenty-four items, which also cover the observed
behavior and appearance assessment during
interview [6].
Objective
The aim of the audit is to look for ways to reduce
BOR of chronic wards. At the same time, we
wish to identify the common reasons of long
inpatient stay in wards in HMBP so that we can
strategize our approach more effectively.
Any recommendation would be based on
standards of care compliance to:
• Psychiatric and mental health services
operational policy (Nov 2011), Ministry
of Health Malaysia (MHM): Section 6.2,
inpatient services and section 6.4
hospital based community psychiatry.
• Mental health act 2001 and mental
health regulation 2010.
• Mentari MOH implementation guideline
2nd edition 2020.
A team of auditors carried out a retrospective
audit looking at numbers and reasons of all
inpatients that are staying longer than 3 months
in hospital Mesra Bukit Padang by the time of
the audit. All patients who are admitted for more
than 3 months are included in the study, while
excluding those who are detained under the court
order CPC section 342, 344 and 348.
Results and Discussion
Data collection was by a team of medical
officers by looking through patients’ clinical
notes, administering a rating scale and filling up
a data collection form. Relevant data to be
collected are:
• Basic demographic information
• Total length of stay in ward
• Medical conditions: Underlying
illnesses
• Psychiatric condition
• Dependency of Activities in Daily
Living (ADL)
• Reasons of keeping patient in ward:
Medical/Psychiatric/Social
• Brief Psychiatric Rating Scale (BPRS)
Additional data of Bed Occupancy Rate (BOR)
and Average Length of Stay (ALOS) of chronic
wards (Ward 4, 5, 9 and 10) are collected by
looking back at the ward census.
This study's data collection period lasted
from May 15, 2023, to June 30, 2023.
The sociodemographic data was analyzed and
described using descriptive statistics such as
frequency, percentage, mean and standard
deviation using IBM SPSS version 28.0. To
facilitate analysis, categorical variables were
transformed into dummy variables. The variables
are checked for normal distribution. Associations
between the variables are analyzed by using Man-Whitney-U test and correlations between
numerical data are analyzed using linear
regression model.
A total of 60 patients are recruited in this study
by sampling all patients that fit the criteria in all
chronic wards. Relevant data are extracted from
their clinical notes and their psychiatric
conditions are assessed by administering BPRS
cross sectionally shown in Table 1. The findings
are tabulated as below:
| Variables |
N=60 |
Mean (sd) |
P-value |
| Yes (%) |
No (%) |
| Length of stay in ward (days) |
2078.50 (5281)* |
|
| Age (years) |
55.06 (12.17) |
| Number of comorbidities |
2 (2)* |
0.209a |
| ADL dependent |
2 (3.3) |
54 (90.0) |
- |
0.657a |
| Primary diagnosis |
0.649a |
| Schizophrenia |
55 (91.7) |
5 (8.3) |
- |
|
| Dementia |
3 (5.0) |
57 (95.0) |
- |
|
| Major depressive disorder |
1 (1.7) |
59 (98.3) |
- |
|
| Schizoaffective disorder |
1 (1.7) |
59 (98.3) |
- |
|
|
Reasons of keeping patients
|
| Medical illness requiring inpatient care |
2 (3.3) |
58 (96.7) |
- |
|
| Maintenance ECT |
6 (10.0) |
54 (90.0) |
- |
|
| Psychiatrically unstable |
9 (15.0) |
51 (85.0) |
- |
|
| Optimization of psychotropic (Clozapine) |
3 (5.0) |
57 (95.0) |
- |
|
| Family uncontactable |
21 (35.0) |
39 (65.0) |
- |
|
| Family refuse to take patient |
24 (40.0) |
36 (60.0) |
- |
|
| Awaiting nursing home |
6 (10.0) |
54 (90.0) |
- |
|
| Other social issues |
8 (13.3) |
52 (86.7) |
- |
|
| BPRS score |
|
|
27.10(3.48) |
|
Note: *Median (IQR), aMan-Whitney-U test, bSpearman’s correlation’s regression model
Table 1. Relevant data are extracted from their clinical notes.
We use the length of stay in ward as an outcome
variable. Schizophrenia is the most common
diagnosis among chronic inpatients (91.7%).
Social reasons are the highest frequency: Family
refuses to take patient (40%), family
uncontactable (35%), awaiting nursing home
(10%) and other social issues (13.3%). There is
noted significant association between
maintenance ECT and length of stay in ward (P
value=0.022). Thus, we can say that the
treatment of maintenance ECT is associated with
longer patient stay in the ward. There is slight
significance noted between family uncontactable
and length of stay in ward (P value=0.049).
There is an association between family uncontactable and increment of length of stay in
ward [7].
There is no association between reasons of
primary diagnosis, medical illness requiring
inpatient’s care, psychiatrically unstable,
optimization of psychotropic (Clozapine), family
refuse to take patient, awaiting nursing home,
other social issues and the length of stay in ward.
There is no correlation between the length of
stay in ward with patients’ BPRS score,
(Spearman’s ρ=0.004, P=0.487). So, there is no
association between patient’s severity of illness
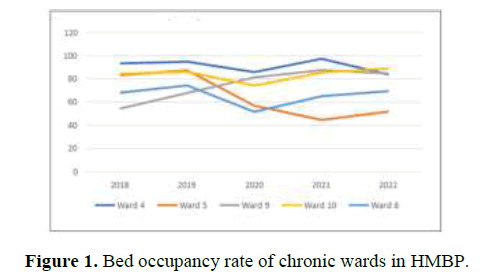
and length of stay in ward (Table 2, Figures 1
and 2). The admission data in chronic wards are
as follows:
| Year |
Gender |
2018 |
2019 |
2020 |
2021 |
2022 |
| Ward 4 |
M |
93.54 |
95.11 |
86.11 |
97.54 |
83.88 |
| Ward 5 |
F |
83.42 |
87.62 |
57.11 |
44.84 |
52.08 |
| Ward 9 |
F |
54.63 |
68.09 |
81.59 |
87.78 |
84.93 |
| Ward 10 |
M |
84.61 |
86.34 |
74.4 |
85.68 |
89.14 |
| Ward 8 |
M |
68.3 |
74.58 |
51.81 |
65.29 |
69.69 |
Table 2. Bed Occupancy Rate (BOR) of chronic wards in HMBP (%).
The BOR of chronic words is as shown above. It
shows that aside from ward 5, all other wards are
static in numbers of patients in ward. Do note
that there is a movement of patients between
ward 8, ward 5 and ward 9 due to the conversion
of roles of wards between them in year 2020.
That may contribute to the changes. Ward 9, 10
and 5 have the highest BOR, which on average
84% for Ward 9 and 10 and 91% for ward 5.
(Ward 9 serves as chronic female ward since
2020, the average BOR for past 3 years is 84%)
[8,9].
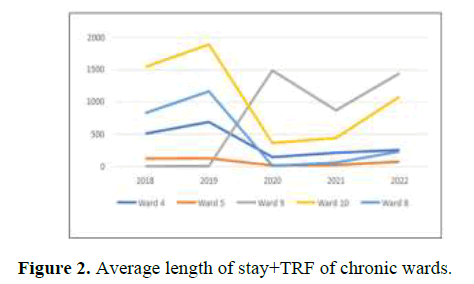
The Average Length of Stay (ALOS) of patients
in chronic wards shows a steady climb across the
graph for the past 3 years. The steep changes in
2019 may be due to the movement of patients
between wards as the ward switch their roles.
The high ALOS in ward 9 and 10 is expected as
those are female and male chronic wards for the
elderly, which most their patients are of
exceptionally long stay and difficult to discharge
(Table 3).
| Year |
Gender |
2018 |
2019 |
2020 |
2021 |
2022 |
| Ward 4 |
M |
512.15 |
694.27 |
152.08 |
217.98 |
262.43 |
| Ward 5 |
F |
130.49 |
133.25 |
22.57 |
30.31 |
82.37 |
| Ward 9 |
F |
11.94 |
12.55 |
1489 |
873.82 |
1446.67 |
| Ward 10 |
M |
1544.17 |
1890.8 |
370.32 |
446.76 |
1084.56 |
| Ward 8 |
M |
831 |
1166.71 |
16.59* |
67.44* |
238.47* |
Table 3: Bed Occupancy Rate (BOR) of chronic wards in HMBP (%).
The association of maintenance ECT and length
of stay in ward is evident, as maintenance ECT
requires patient to come to HMBP as frequent as
weekly for the treatment and there are no
hospitals within the cluster to offer such service
yet. Such treatment frequency brings expected
logistic issues, especially for those who live far
away in other cities. There is a need for more
centers offering this service to bring it closer to
the people. However, before such step even
become feasible, more psychiatry units need to
be established first, which will require resources
in all forms [10].
The reason of ‘family uncontactable’ being
associated with length of stay in ward can be
justified by the non-existence of any social
support available for these patients. Different
than those of ‘family refused to take patient’ who
still has family member around for the hospital
staffs to engage with, these patients have no one
for the hospital staffs to contact with. There is
also no agency that would provide
accommodation for them because of the lack of a
legal confidant. Thus, the increment of their
length of stay in ward is almost inevitable [11].
One issue worth highlighting is that there is no
association noted between the severity of illness (BPRS score) and the length of stay. This
supports the notion that severity of their
psychiatric illness has no influence on their
length of stay in ward. Some patients in chronic
wards are psychiatrically stable but stay longer
than others. This is not cost effective as there are
better ways to help such patients to be
independent in the community, while conserving
our hospital resources for those who need it
more. Such strategies will be discussed below.
Social reasons are the most common reason for
patients unable to be discharged from HMBP.
The data shows a discrepancy in between the
reasons frequency (%) and their significance of
association (P-value). Such discrepancy suggests
that there are more patients with reasons that
without significance are being kept longer in
chronic ward. Urgency is needed to address this
issue due to the impact it can have on our
psychiatry service, such as budgeting, facility
usage and service quality. Although it is a
common issue found in all mental institutions in
Malaysia, it is worth reminding ourselves that it
is a preventable matter [12].
The reluctancy of family members to bring the
patients home suggests stigmatization. The lack
of understanding and stigma from family members are main contributing factors for them
to become reluctant to care for their loved ones
at home. The effort to engage with the families
has been done with the help of social workers, by
repeating phone calls and family tracing but
there is no improvement in the BOR [13].
Although addressing stigmatization objectively
will require another research, the authors hope to
include this topic in discussion to look for
possible countermeasures for this serious
phenomenon. Another issue of concern is the
costs of in-patient care. Based on monthly report
by finance unit, for April 2023, HMBP has
recorded total admission of 4582 patient days.
For the cost of inpatient treatment alone, HMBP
spends a total of RM 2.7 million in just a month.
This number, when compared to outpatient costs,
which is RM 280,000 for 1,660 patients in April
2023, an almost difference of 10 fold is observed
[14]. Considering that there are patients who are
psychiatrically stable, who do not require active
psychiatric intervention and just for continuation
of medication, such costs of inpatient care may
not be cost effective in the service.
Recommendation
There is always a concern of patients being
unwell when they are discharged without a
caretaker. So, mental institutions adopted the
concept of having chronic wards for
rehabilitation purpose. With the increment of
needs for accommodating the mentally ill who
are having social difficulties, much effort has
done to expand the infrastructure as we seen in
other centers such as hospital Permai and
Bahagia. The option of expansion of chronic
wards is although doable, but not cost effective.
By allowing more psychiatric patients to stay in
ward, it requires more budgets to sustain their
inpatient care, be it resources of workforce,
medical equipment and daily needs like food and
utilities. With the expansion of available services
and subspecialties, the national budget should be
well spent on enhancing the quality of care
towards our patients.
Many countries, including WHO, have proposed
the idea of de-institutionalization since more
than 50 years ago. However, there are mixed
reports regarding its outcome, as each report
offers different perspectives: clinical,
socioeconomical and ethical points of view.
However, it consistently shows that with a good
well planned community strategy, much benefit
can be gained even from the socioeconomical point of view (Knapp, et al., 2010). Based on a
systemic review by McPherson et al in 2018,
there is a noted benefits in supported
accommodation that it improved appropriate use
of service and reduction in hospitalization among
de-institutionalized patients. Thus, we propose a
program of supported accommodation, with
Hospital Permai Johor Bahru as a reference
point.
Hospital Permai has implemented supported
accommodation for patients who are deemed
psychiatrically stable and fit to live by
themselves. As compared to the inpatient chronic
residency, which consist of having patients under
hospital care staying inside an apartment built
within hospital grounds, supported
accommodation involves patient living in
accommodation units outside the hospital, which
premises mostly are given by local authorities
who support the program. Patients are required
to work, often by supported employment, to pay
for their rent (amount about RM70) and daily
expenses. The community psychiatry team
would visit them regularly to check on their
progress and support the local communities by
giving out education in order to help to reduce
stigma towards the patient. So far, as when this
report is written, seventeen patients in HPJB
chronic wards were successfully gone through
the program, sustaining themselves with a job
within the community. One strategy currently
underway is to transfer chronic patients who
require constant medical care and psychiatrically
stable to the district hospital as lodgers. This is
done out of the need of bed vacancy and it is not
cost effective as other hospitals too will share the
cost burden.
Another strategy is to lower the admission rates
altogether, by improving our service. A stronger
therapeutic alliance is needed between clinician
and the family members. Psychoeducation is
important in reducing stigmatization. Study has
shown that it improvesthe long-term outcome
among patients of schizophrenia, by having a
reduction of relapse rate of 50-60% (McFarlane,
2016). We suggest implementing a structured
psychoeducation module for the patients and
family. The Ministry of health provided a
structured psychoeducation module for family
and patients, which comprises 8 components.
However, there is a constant need for resources
to have the facility and staff to routinely
administer such modules effectively. There is a
need to establish more treatment centers available within the area. Treatment gap refers to
the difference between those who require
treatment and those who got treated. In
psychiatry, is has known to be a worldwide issue
as there are huge difficulty for the mentally ill to
get the help they need. Such difficulty will bring
delay in treatment, resulting in adverse outcome.
With a wide area of coverage handled by HMBP,
it receives psychiatry patients with the need of
admission from areas from Beaufort all the way
to Kudat (Distance of 400 km). Out of the
cluster’s hospitals, there’s only HMBP who are
equipped with psychiatry ward at the moment of
this report. So, much urgency is needed to have
other centers within the cluster to be equipped
with psychiatry units, to reduce the patient load
in HMBP.
Approaches like community outreach are also
important in reducing the need for psychiatric
admission. A recent study done in Kuala Lumpur
has shown that a good outreach strategy could
reduce patient readmission rate. Community
outreach encompasses mental health promotion
to the public, educating primary caregivers,
preparing the public health sector the skills
needed to identify the illnesses, as well as
working with different agencies to provide
support to those who are affected. Such an
approach has been implemented in HMBP,
which is having a community mental health
center focusing on rehabilitation called
‘Mentari.’ Mentari program has been
implemented in the national practice since The
Eleventh Malaysia Plan (EMP-2016-2020). The
aim is to have a community center that focuses
on rehabilitation of the mentally ill and reduce
the illness burden, by giving out supported
employment, psychosocial rehabilitation,
sheltered workshop, home visit and social
enterprise. It is also focused on reducing stigma
within the community. However, as of now, only
one Mentari center is available on the west coast
of Sabah and it is stationed within HMBP
ground. The team urges the need to establish
more community mental health centers.
Good alliances with other agencies are important
as well. There is a need to clarify that with deinstitutionalization,
the economic burden for
patients with great disability will be shared
between agencies such as healthcare, social
welfare, as well as families. So, there must be a
good collaboration between agencies to achieve
cost effectiveness. Hospital social welfare that
are engaging with the family members are facing
difficulty due to lacking resources. The options presented for them are limited, as financial aid
and supported accommodations options are
scarce and nursing homes are mostly run by the
private sectors or NGO, thus incurring a demand
in price to the families. We suggest a frequent
discussion with the state social welfare and
NGOs to discuss a means of collaboration to
maximize each other’s role in service.
Conclusion
• Social factors are the most common
reason for chronic inpatient stay in
HMBP.
• Severity of psychiatric illness is not
associated with the length of stay of
chronic inpatients.
• Cost efficiency demands steps to be
taken to reduce the inpatient load, such
as: Implementation of psychoeducation
module; establishing new Mentari
centers and outreach strategies.
• Supported accommodation.
Limitations
The author acknowledges that assessment
towards the caregiver’s perspective such as
their stigmatization would provide a more
concrete data, but there’s a difficulty in
engaging family members of patients in chronic
wards as they are usually difficult to meet with
clinicians. There might exist an inter rater
variability when administering BPRS by
different clinicians. A brief meeting and
teaching have been conducted between the
clinicians and they are instructed to comply
with the BPRS manual. The recommendations
are for reference purposes for the hospital
administrators as the author is not stationed on
site.
Acknowledgment
The Authors would like to thank Hospital
Mesra Bukit Padang for allowing the audit to
be taken place and the cooperation from the
admin and staff during the audit period.
Declaration of Interest
The authors declare that there is no conflict of
interest regarding the publication of this article.
This research did not receive any specific grant
from funding agencies in the public,
commercial or not-for- profit sectors. This audit
receives no funding or sponsors from any party.
Ethical Issues
The project is pending approval from the
Malaysia Research Ethical Committee (MREC)
approval.
References
- Chow WS, Priebe S. Understanding psychiatric institutionalization: A conceptual review. BMC Psychiatry. 2013;13(1):1-4.
[Crossref] [Google Scholar] [PubMed]
- Shen GC, Snowden LR. Institutionalization of deinstitutionalization: A cross-national analysis of mental health system reform. International Journal of Mental Health Systems. 2014;8(6):1-23.
[Crossref] [Google Scholar] [PubMed]
- McDaid D, Knapp M, Raja S. Barriers in the mind: Promoting an economic case for mental health in low-and middle-income countries. World Psychiatry. 2008;7(2):79-86.
[Crossref] [Google Scholar] [PubMed]
- Raaj S, Navanathan S, Tharmaselan M, Lally J. Mental disorders in Malaysia: An increase in lifetime prevalence. B J Psych International. 2021;18(4):25-30.
[Crossref] [Google Scholar] [PubMed]
- Hofmann AB, Schmid HM, Jabat M, Brackmann N, Noboa V, et al. Utility and validity of the Brief Psychiatric Rating Scale (BPRS) as a transdiagnostic scale. Psychiatry Research. 2022;314(143):614-659.
[Crossref] [Google Scholar] [PubMed]
- Overall JE, Gorham DR. The brief psychiatric rating scale. Psychological Reports. 1962;10(3):799-812.
[Crossref] [Google Scholar]
- Shafer A. Meta-analysis of the brief psychiatric rating scale factor structure. Psychological Assessment. 2005;17(3):324.
[Crossref] [Google Scholar] [PubMed]
- Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the Brief Psychiatric Rating Scale:" the drift busters." International Journal of Methods in Psychiatric Research. 1993;11(8):77-83.
[Google Scholar]
- Monnapula-Mazabane P, Petersen I. Mental health stigma experiences among caregivers and service users in South Africa: A qualitative investigation. Current Psychology. 2023;42(11):9427-9439.
[Crossref] [Google Scholar] [PubMed]
- McPherson P, Krotofil J, Killaspy H. Mental health supported accommodation services: A systematic review of mental health and psychosocial outcomes. BMC Psychiatry. 2018;18(6):1-5.
[Crossref] [Google Scholar] [PubMed]
- Knapp M, Beecham J, McDaid D, Matosevic T, Smith M. The economic consequences of deinstitutionalization of mental health services: lessons from a systematic review of European experience. Health and Social Care in the Community. 2011;19(5):113-125.
[Crossref] [Google Scholar] [PubMed]
- McFarlane WR. Family interventions for schizophrenia and the psychoses: A review. Family Process. 2016;55(24):460-482.
[Crossref] [Google Scholar] [PubMed]
- Dahlan R, Midin M, Sidi H, Maniam T. Hospital-based community psychiatric service for patients with schizophrenia in K uala L umpur: A 1 year follow up study of re-hospitalization. Asia Pacific Psychiatry. 2013;5(2):127-133.
[Crossref] [Google Scholar] [PubMed]
- Fekadu A, Medhin G, Lund C, DeSilva M, Selamu M, et al. The psychosis treatment gap and its consequences in rural Ethiopia. BMC Psychiatry. 2019;19(8):1-11.
[Crossref] [Google Scholar] [PubMed]
Citation: Clinical Audit Report: Number, Reasons and Indication of Inpatient in Chronic Wards in Hospital Mesra Bukit Padang, Sabah, Malaysia. ASEAN Journal of Psychiatry, Vol. 25 (1) January, 2024; 1-8.