Abstract
It is known that a large proportion of children and adults have been exposed to significant trauma at some stage in their lives and that childhood trauma is associated with mental and physical ill-health. There is an accumulating literature that shows a high proportion of the mentally ill report childhood abuse and neglect. Studies showing evidence of a strong association of childhood trauma histories and specific mental illnesses, high prevalence of childhood trauma in psychiatric out-patients and as a result, higher utilization of mental health services, are cited. The evidence of association of childhood trauma and the serious mental illnesses is compelling and the ACES’ study of the past three decades have emphasised its impact. The limitations of these studies are openly considered, but in spite of the immense volume of literature on the subject, there continues to be a widening gap between clinical and biological research with serious therapeutic implications. Most of the illnesses we deal with in psychiatry have neurodevelopmental origins, which underscore the importance of focussing on early life as an age to understand how non-heritable factors interact with the genome to confer vulnerability. It is suggested that if psychiatry recognizes early childhood trauma in patients’ histories, it may help modify the course and possibly the treatment outcome of mental illnesses, particularly mood disorders. This course of action would enable more rigorous research, encourage routine practice of taking into account ACE’s during assessment and consider trauma in the management of psychiatric illnesses across all service systems, irrespective of diagnosis.
Keywords
Childhood Trauma; ACEs; Mental Health; Management; Psychiatry
Introduction
Approximately 2.5 million Australian adults (13%) have experienced abuse during their childhood. This includes 1.6 million adults (8.5%) who experienced childhood physical abuse and 1.4 million adults who experienced childhood sexual abuse. The average age at which the first incident of abuse occurred was 8.8 years for persons who experienced sexual abuse only, 8.1 years for persons who experienced physical abuse only and 6.8 years for persons who experienced both physical and sexual abuse [1].
12% of men who had experienced childhood abuse had a psychological disability compared with 3% who did not experience childhood abuse; 29% had a physical disability compared with 19% who did not experience childhood abuse and in women 35% had a physical disability compared with 4% who did not experience childhood abuse and 13% of women had a psychological disability compared with 4% who did not experience childhood abuse (Australian Bureau of Statistics 2019).
The worldwide average trauma exposure rate is 69% for children and adults and almost 40% of the population surveyed in 21 countries were found to have suffered adverse childhood experiences. It is confronting indeed when one sees a patient who has been in the mental health system for decades and who for the first time has the experience of a clinician who is interested in their trauma history [2].
Literature Review
Child maltreatment and its association with mental illness
Over the past few decades childhood adversities have been one of the most consistently documented risk factors for psychiatric disorders. Half of all lifetime mental health disorders emerge in childhood and one in seven Australian children experience a mental health disorder in any given year. Of all maltreatment types, emotional abuse impacts mental health in wide-ranging ways and appears to be a transdiagnostic risk factor for several psychiatric disorders including treatment resistant depression [3].
Child maltreatment and its association with adult depressive disorders
Summarizing the literature investigating the effects of childhood maltreatment on disease vulnerability for mood disorders, specifically cross-sectional and more recent longitudinal studies demonstrated that childhood maltreatment is more prevalent and is associated with increased risk for first mood episode, episode recurrence, greater comorbidities, increased risk for suicidal ideation and attempts in individuals with mood disorders [4]. Epidemiological and clinical studies provide evidence that childhood maltreatment may negatively affect not only the lifetime risk of depression but also clinically relevant measures of depression, such as course of illness and treatment outcome, as suggested by a meta-analysis of 16 epidemiological studies (23,544 participants) which showed that childhood maltreatment was associated with an elevated risk of developing recurrent and persistent depressive episodes (odds ratio=2.27, 95% confidence interval CI=1.80-2.87). In addition, meta-analysis of 10 clinical trials (3,098 participants) by the same group revealed that childhood maltreatment was associated with lack of response or remission during treatment for depression (odds ratio=1.43, 95% CI=1.11-1.83) and meta-regression analyses suggested that the results were not significantly affected by publication bias, choice of outcome measure, inclusion of prevalence or incidence samples, study quality, age of sample or lifetime prevalence of depression [5].
Child maltreatment and its association with personality disorders
Adults with a history of child abuse and neglect (indicated by records or self-report) were found to have a fourfold increase in personality disorders relative to those with no such history. The Child trauma questionnaire administered to a cohort of patients with treatment resistant depression referred to a specialist psychotherapy unit found that emotional and sexual abuse were common as was physical abuse and neglect, however emotional abuse rated highest and a high degree of personality pathology was present [6]. Seventy five percent of all psychiatric disorders present before the age of 24 years and cumulative childhood trauma exposure to age 16 years was found to be associated with higher rates of adult psychiatric disorders and poorer functional outcomes, including key outcomes that indicate a significantly disrupted transition to adulthood. In a large community study documented child sexual abuse was associated with borderline personality disorder symptoms, documented physical abuse with antisocial and depressive symptoms and childhood neglect was associated with antisocial, avoidant, borderline, narcissistic and passive-aggressive personality disorders. Records were used that corroborated abuse, therefore retrospective data was not relied upon and association with symptoms was found but not association with disorders [7].
Increasing rates of non-suicidal self-injury in the context of traumatic exposure continues to baffle clinicians, as those diagnosed with a personality disorder frequently have personality traits of two or more different personality disorders, particularly those with borderline personality, complicated by the presence of PTSD or complex PTSD. A comprehensive meta-analysis of childhood maltreatment (over-all sexual abuse, physical abuse and neglect, emotional abuse and neglect) in association with non-suicidal self-injury revealed that overall childhood maltreatment was associated with non-suicidal self-injury across multiple maltreatment subtypes and stronger associations were found with non-suicidal self-injury in non-clinical samples [8].
In routine clinical practice, borderline personality disorder, which is one of the most researched of all personality disorders, often presents with such complexity as to merit multiple axis 1 diagnoses. These people report more types and severities of abuse, more frequent emergency room visits, hospital admissions, higher utilization of mental health services, increased substance abuse and episodes of self-harm, suicide attempts, higher number of mental health professionals caring for them, visits to therapists and utilization of pharmacotherapy. There is a complex inter-relationship between their history of abuse and their clinical presentations which must be attended to if their symptoms are to remit.
Until recently, personality disorders were considered separately from other mental disorders as an intractable state with a primarily environmental aetiology and rather refractory to treatment [9].
Personality disorders are widely recognized as a major mental health disorder that is associated with severe psychosocial dysfunction and reduced quality of life. Personality disorders are developmental disorders with onset in childhood and adolescence-they do not suddenly emerge at 18 years of age-a lifelong process if intervention is not offered early. Early childhood trauma affects the development of personality. Personality disorders when present with an axis 1 disorder make for increased complexity both in diagnosis as well as in treatment, particularly compliance and response to medication and the general functionality of the patient (Figure 1) [10].
Child maltreatment and its association with other major mental illnesses
Child abuse and neglect alters the trajectory of most mental illnesses. A review on the role of childhood trauma in bipolar disorders contributed a new understanding of the negative effects of early life stress, as well as setting childhood trauma in a biological context of susceptibility and novel long-term pathophysiological consequences in bipolar disorder [11]. Childhood traumatic events are risk factors for developing bipolar disorder, in addition to a more severe clinical presentation over time; primarily an earlier age of onset and an increased risk of suicide attempt and substance abuse. Relevant studies identified via medline and PsycINFO databases published up to and including July 2015 were reviewed and found a high proportion of children who had experienced any form of childhood maltreatment were significantly more likely to self-report generalized anxiety disorder, post-traumatic stress disorder or major depression than those without such a history. Similarly, studies found self-reported child abuse and neglect were related more generally to psychopathology in psychiatric samples, in suicide and suicidal behaviour and that clinically significant childhood maltreatment is relatively common in individuals with Body Dysmorphic Disorder (BDD), where certain types of abuse and neglect appear modestly associated with BDD symptom severity and with gender and suicidality [12].
Child maltreatment and its effects on the brain
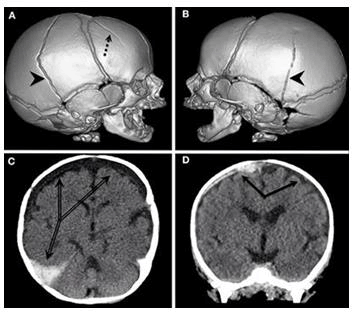
Child abuse and neglect occur in the context of a child’s brain development and their potential effects on developing brain structure can help explain the onset of certain negative outcomes, though to extrapolate this further is difficult as a number of confounding factors present themselves as the child continues to grow. Many studies of the consequences of abuse and neglect have been conducted with methodologies ranging from prospective to retrospective, from observational measures to self-report and from experimental to case controlled design to no-control design. However, it would not be desirable or possible to obtain proof by randomly assigning children to abusive, neglectful or caring environments (Figure 2) [13].
The developing brain is characterised by a high degree of neural plasticity and while allowing for the refinement of neurocircuitry that is specifically tuned to the demands of the surrounding environment, it also makes the developing brain particularly vulnerable to any perturbation to maturing systems which disrupt neural circuits resulting in long term consequences for both cognitive and emotional memory systems. Dysregulation of emotional memory systems are important components of many psychiatric disorders and there is increasing evidence that childhood adversity is associated with altered activity of the HPA axis [14]. The findings of developmental neuroscience have improved our understanding of the early-life factors that confer risk for the development of psychiatric disorders and underscore the importance of studying early development at multiple levels to better understand mechanisms that predispose to the emergence of psychopathology.
Discussion
Child maltreatment, the global burden of disease and treatment response
It is established that childhood maltreatment has devastating consequences in the context of health and disease. Research has begun to elucidate mechanisms underlying the link between childhood abuse and neglect and medical, including psychiatric outcomes. It is associated with an earlier age of onset, a more severe clinical course and poorer treatment response to pharmacotherapy or psychotherapy [15].
Joint association of 12 childhood adversities in first onset of 20 DSM-1V disorders in world mental health in 21 countries, where a total of 51,945 adults showed that childhood adversities often co-occur and that clusters of childhood adversities associated with maladaptive family functioning are linked with the highest risk of mental disorders and has important implications for intervention, namely reduced exposure to all childhood adversities rather than a single adversity. Psychiatric disorders constitute a higher percentage of the global burden of disease than cancer and other diseases.
Child maltreatment, diagnostic dilemmas and treatment resistance
The mainstream notion of disease in psychiatry aims to discover specific mental disorders and to demarcate normality from abnormality, by eliciting certain signs and symptoms. This approach disregards individual lifetime experiences, the confounding effects and complexity of trauma and therefore profound implications for treatment and prognosis.
The differential diagnosis between emotional dysregulation of the borderline personality, which is generally on a background of childhood trauma and that of bipolar affective disorder is one of those most recent and difficult scenarios we now encounter.
A diagnostic dilemma is often created by increasing complexity and treatment resistance due to the failure of medications and other physical treatments being ineffective in the treatment of complex trauma. The confusion that exists between diagnosis of a psychotic disorder versus a dissociative disorder is now all too common and depends largely on the artificial division of psychiatrists as biological/psychodynamic. This is in sharp contrast to situations where the possibility of a major contributory physical factor is suspected in patients with depression or psychosis, organicity is recognised, investigated and taken into account when treating the mental illness.
The prevailing rates of childhood abuse and neglect in the mentally ill tend to be under-estimated for several reasons: the tendency for persons to avoid disclosing due to perceived stigma, the acute mental illness takes precedence and prevents history taking of trauma, and neglect on the part of the clinician to acknowledge childhood trauma’s association with mental illness. Although a history of trauma is sometimes difficult to elicit, it can be suspected from the patient’s mental state i.e. a lack of continuity, coherence and clarity, in the absence of psychosis. There is always the possibility of trauma being disclosed if the clinician is open to it. The role of trauma in treatment resistance i.e. non-responsive depression to several medications, combinations of medications, trans-cranial magnetic stimulation and ECT, is ignored in the literature.
Conclusion
Gardner and Kleinman urge for more research that includes the brain and mind i.e. biology and psychology, stating that “biological psychiatry has thus far failed to produce a comprehensive theoretical model of any major psychiatric disorder.” There is a large gap at present between clinical observations of the part early childhood trauma plays and the relative paucity or even absence of trauma mentioned in treatment guidelines for major mental illnesses. Clinicians should be alert to childhood abuse in the severely mental ill, as the consequences may contribute to the clinical picture and may require special attention and measures to be taken into treatment. More research is needed to improve our knowledge of the relationship between childhood trauma, genetic predisposition and the clinical picture in patients with severe mental illness.
Though specific associations have been established, causality cannot be assumed but do merit research, in order to disentangle the effects of child maltreatment from other conditions and from environmental mechanisms that mediate the association between abuse, neglect and their consequences. The research of the past three decades and the current state of knowledge about the consequences for mental health of early trauma (sexual, physical, emotional abuse and neglect) begs psychiatry to take heed, as a sizable proportion of victims of childhood abuse present to medical and psychiatric systems and receive various diagnoses which do not necessarily refer to their trauma. We must break our silence.
References
- Aas M, Henry C, Andreassen OA, Bellivier F, Melle I, et al. The role of childhood trauma in bipolar disorders. Int J Bipolar Disor. 2016; 4(1):1-10.
[Crossref] [Google Scholar] [PubMed]
- Copeland WE, Shanahan L, Hinesley J, Chan RF, Aberg KA, et al. Association of childhood trauma exposure with adult psychiatric disorders and functional outcomes. JAMA Netw Open. 2018;1(7):184493.
[Crossref] [Google Scholar] [PubMed]
- Didie ER, Tortolani CC, Pope CG, Menard W, Fay C, et al. Childhood abuse and neglect in body dysmorphic disorder. Child Abuse Negl. 2006;30(10):1105-1115.
[Crossref] [Google Scholar] [PubMed]
- Gardner C, Kleinman A. Medicine and the mind-the consequences of psychiatry’s identity crisis. N Engl J Med. 2019;381(18):1697-1699.
[Crossref] [Google Scholar] [PubMed]
- Johnson JG, Cohen P, Brown J, Smailes EM, Bernstein DP. Childhood maltreatment increases risk for personality disorders during early adulthood. Arch Gener Psych. 1999;56(7):600-666.
[Crossref] [Google Scholar] [PubMed]
- Kessler RC, Avenevoli S, McLaughlin KA, Green JG, Lakoma MD, et al. Lifetime co-morbidity of DSM-IV disorders in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A). Psychol Med. 2012;42(9):1997-2010.
[Crossref] [Google Scholar] [PubMed]
- Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Ann Rev Public Health. 2008;29:115-129.
[Crossref] [Google Scholar] [PubMed]
- Koenen KC, Ratanatharathorn A, Ng L, McLaughlin KA, Bromet EJ, et al. Post-traumatic stress disorder in the world mental health surveys. Psychol Med. 2017;47(13):2260-2274.
[Crossref] [Google Scholar] [PubMed]
- Lippard ET, Nemeroff CB. The devastating clinical consequences of child abuse and neglect: Increased disease vulnerability and poor treatment response in mood disorders. Am J Psychiatr. 2020;177(1):20-36.
[Crossref] [Google Scholar] [PubMed]
- Liu RT, Scopelliti KM, Pittman SK, Zamora AS. Childhood maltreatment and non-suicidal self-injury: A systematic review and meta‑analysis. Lancet Psych. 2018;5(1):51‑64.
[Crossref] [Google Scholar] [PubMed]
- Meyer HC, Lee FS. Translating developmental neuroscience to understand risk for psychiatric disorders.Am J Psychiatr. 2019;176(3):179-185.
[Crossref] [Google Scholar] [PubMed]
- Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta‑analysis. Am J Psych. 2012;16(2):141-151.
[Crossref] [Google Scholar] [PubMed]
- Nemeroff CB. Paradise lost: The neuro-biological and clinical consequences of child abuse and neglect. Neuro. 2016;89(5):892-909.
[Crossref] [Google Scholar] [PubMed]
- Pandey R, Gupta S, Upadhyay A, Gupta RP, Shukla M, et al. Childhood maltreatment and its mental health consequences among Indian adolescents with a history of child work. Aust N Z J Psych. 2020;54(5):496-508.
[Crossref] [Google Scholar] [PubMed]
- Stevenson J, Haliburn J, Halovic S. Trauma, personality disorders and chronic depression: The role of the conversational model of psychodynamic psychotherapy in treatment resistant depression. Psychonal Psychother. 2016;30(1):23-41.
[Google Scholar]