Introduction
The Pre Exposure Prevention (PrEP) program had been launched in Vietnam with a goal to fast track targets of 90-90-90 by 2023. PrEP has been proven to be effective and is recommended to reduce the rate of HIV infection [1,2]. The PrEP program was first implemented in March 2017 in Ho Chi Minh City. By 2022, there were nearly 11,686 Men having Sex with Men (MSM) who was receiving PrEP counselling and treatment [3].
In Vietnam, a Community Based Organization (CBO) includes a variety of local organizations with staff that are familiar with the needs of a particular high risk population or community (e.g. transgender/people living with HIV, etc.). In HIV/AIDS prevention, the interventions offered by the CBO are most relevant with a frontline role and have been found to be of proven effective in HIV/AIDS prevention, early detection and complete support for HIV patients [4-7].
In Vietnam, since 2011, HIV/AIDS prevention and control activities have had strong participation from CBOs, focusing mainly on high risk groups including: MSM, transgender women, Injecting Drug Users (IDUs), and female sex workers. The application of a CBO model in HIV infection prevention has been quite effective with detection rates of new positive cases up to 6%-7% of the total number of tested persons.
The COVID-19 pandemic had disrupted the care continuum services in various settings. The restrictions in response to the pandemic made the functioning of the CBOs challenging. Resource shortages, low staff morale, and disruption to patient cantered service provision were listed as the key challenges for the CBOs. It was extremely important to adjust the delivery and approach strategies, coordinate with stakeholders to support patients on time and in a comprehensive manner. This was especially relevant in context of the PrEP and ARV clients who need to use medication every day are at high risk of contracting COVID-19. Driven by the necessity and need to innovate, the CBOs also devised new ways to ensure the provision of services to those in need in the last few years [8].
It has been reported in the previous literature that the measurable effectiveness of CBOs is yet to be realized [9]. The disruption of HIV/AIDS related services in Vietnam during the pandemic has been reported [10]. It has been recommended that the research that focuses on the community can be utilized to monitor how much COVID-19 is affecting CBO operations, provider actions, and client experiences and results. However, currently there are no published reports on this theme from the South East Asia region.
The current study aimed to assess the role of community based organizations in supporting ARV and PrEP before and during COVID-19 in Ho Chi Minh City and Dong Nai provinces in Vietnam. This would help document good practice examples from this experience as well as help identify the challenges that need to be addressed in the future.
Materials and Methods
Objectives of the operational research study
The current operational research was planned with the objectives of describing the status of treatment adherence and factors (such as baseline characteristics, pathological characteristics) between the group of clients transferred by the CBO and the group of walk in clients for PrEP and ARV; determining client's satisfaction with the CBO's PrEP and ARV treatment support services; exploring satisfaction and demand of clients for the CBO's PrEP support and HIV management; exploring satisfaction and demand of stakeholders (from the disease control centers, health centers, PrEP and ARV clinics) for the CBO's PrEP support and HIV management; finding different ways to access and the support of treatment between clients transferred by the CBO and walk in clients for PrEP and ARV.
Study setting
The study was carried out at the outpatient clinics providing PrEP and ARV in Ho Chi Minh City and Dong Nai provinces in Vietnam.
Study design
This operational research was carried out using mixed methods. The quantitative part of the study included a survey and extraction of the medical records of clients on ARV and PrEP registered between 1st November 2021 to 31st December 2021. Those aged 18 years or older and received services (PrEP or HIV) between October 1, 2020, and June 30, 2021, and willing to participate in the study were included. Those clients who were not able to participate were excluded from the study.
Sampling and sample size
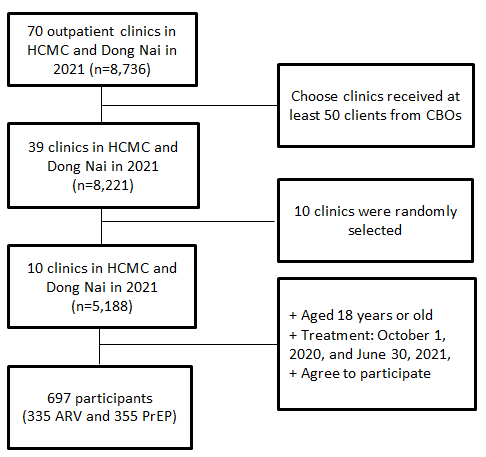
The quantitative study used a single stage cluster sampling method. A total of 70 outpatient clinics in HCMC and Dong Nai province were listed. Out of these, those clinics that received at least 50 clients from the CBOs were retained. This led to a total of 25 outpatient clinics in HCMC and 14 in Dong Nai provinces. From these clinics a total of 10 clinics were randomly selected. This resulted in 6 clinics from HCMC and 4 from Dong Nai provinces. All the clients registered at these clinics were listed and a total of 697 clients meeting the study criteria were randomly selected (Figure 1).
Assessment tools
The information was gathered using the existing medical records of the clients as well as face to face interviews. A predesigned semi structured questionnaire that was prepared and approved by a multidisciplinary team of researchers was used for this purpose. The questionnaire included questions on general socio demographic and clinical profile (14 questions), characteristics of PrEP/ARV treatment (9 questions), Morisky Medication Adherence Scale (MMAS-8 Scale) (8 questions), understanding of CBO (11 questions), Client Satisfaction Questionnaire (CSQ-8) (8 questions), PrEP/ARV treatment during COVID-19 (4 questions).
Therapeutic adherence was calculated based on the Morisky medication adherence scale. This eight item tool is a structured self-report measure of medication taking behaviour that has been widely used in various cultures. The overall MMAS-8 scale ranges from 0 to 8. The adherence was classified into 2 levels: High adherence (6-8 points) and low adherence (<6 points) [11].
The Client Satisfaction Questionnaire (CSQ-8), which has 8 items measures client satisfaction with services. The CSQ-8 items were chosen based on factor analysis after mental health professionals rated a number of items that might be connected to client satisfaction. The CSQ-8 measures general satisfaction with services in a uniform manner because it is unidimensional [12].
Statistical analysis
The data were analyzed using the STATA software, version 10.0. Description of frequencies and percentages for socio demographic characteristic variables and treatment was done.
Logistic regression was used with estimated Odds Ratio (OR) with corresponding 95% Confidence Intervals (95% CI) to test the association between socio demographic characteristics, treatment characteristics, and treatment adherence. The p<0.05 value was considered as the threshold of statistical significance.
Results
A total of 697 clients were recruited, 7 clients (1%) were rejected due to not meeting the criteria for selection. The final analysis sample had 690 clients, including 335 ARV clients and 355 PrEP clients.
The socio demographic characteristics of ARV and PrEP clients according to clients transferred by the CBO and walk in clients are given in Table 1. The majority of ARV and PrEP clients were young men between the ages of 20-29, accounting for more than 50%. Clients transferred by a CBO tended to be younger than walk in clients. The education level of PrEP clients was higher than that of ARV clients. Also, PrEP clients transferred by a CBO were more educated than the group of walk in clients. ARV clients transferred by the CBO had a lower rate of financial autonomy than the group of walk in clients (76.2% versus 85.0%).
| Socio-demographic characteristics** |
ARV1 (n=335) (n, %) |
PrEP1 (n=355) (n, %) |
| CBO (n=168) |
Walk in (n=167) |
CBO (n=185) |
Walk in (n=170) |
| Age* |
26 (22-30) |
29 (24-35) |
26 (22-31) |
26 (22-31) |
| Age group |
| 15-19 |
13 (7.7) |
6 (3.6) |
12 (6.5) |
10 (5.9) |
| 20-24 |
63 (37.5) |
36 (21.6) |
67 (36.2) |
55 (32.3) |
| 25-29 |
47 (28.0) |
52 (31.1) |
51 (27.6) |
57 (33.5) |
| 30-34 |
21 (12.5) |
21 (12.6) |
31 (16.7) |
27 (15.9) |
| ≥ 35 |
24 (14.3) |
52 (31.1) |
24 (13.0) |
21 (12.4) |
| Gender |
| Male |
161 (95.8) |
154 (92.2) |
180 (97.3) |
163 (95.9) |
| Female |
5 (3.0) |
12 (7.2) |
3 (1.6) |
6 (3.5) |
| Transgender women |
2 (1.2) |
1 (0.6) |
2 (1.1) |
1 (0.6) |
| Education level |
| Primary school |
9 (5.4) |
12 (7.2) |
3 (1.6) |
2 (1.2) |
| Junior high school |
30 (17.8) |
23 (13.8) |
19 (10.3) |
9 (5.3) |
| High school |
51 (30.4) |
61 (36.5) |
30 (16.2) |
28 (16.5) |
| Above high school |
78 (46.4) |
71 (42.5) |
133 (71.9) |
131 (77.1) |
| Marital status |
| Single |
150 (89.3) |
123 (73.6) |
163 (88.1) |
159 (93.4) |
| Married |
12 (7.1) |
31 (18.6) |
11 (5.9) |
7 (4.2) |
| Living with a partner/lover |
3 (1.8) |
5 (3.0) |
9 (4.9) |
4 (2.4) |
| Separated/divorced/widowed |
3 (1.8) |
8 (4.8) |
2 (1.1) |
0 (0.0) |
| Financial status |
| Full autonomy |
128 (76.2) |
142 (85.0) |
148 (80.0) |
145 (85.3) |
| Partial autonomy |
26 (15.5) |
15 (9.0) |
32 (17.3) |
19 (11.2) |
| Indigent |
14 (8.3) |
10 (6.0) |
5 (2.7) |
6 (3.5) |
| Occupation |
| Office workers |
44 (26.2) |
48 (28.6) |
71 (38.4) |
75 (44.1) |
| Worker/laborer |
36 (21.4) |
38 (22.8) |
25 (13.5) |
14 (8.2) |
| Freelancer |
41 (24.4) |
26 (15.6) |
36 (19.5) |
31 (18.2) |
| Sales/business |
16 (9.5) |
31 (18.6) |
15 (8.1) |
8 (4.7) |
| Student |
16 (9.5) |
8 (4.8) |
30 (16.2) |
30 (17.7) |
| Unemployed |
6 (3.6) |
10 (6.0) |
0 (0.0) |
0 (0.0) |
| Service staff |
9 (5.4) |
6 (3.6) |
8 (4.3) |
12 (7.1) |
Note: *Median (interquartile range); **Collected via client response;
1Notes: ARV: Antiretroviral; PrEP: Pre-exposure Prophylaxis.
Table 1. Socio-demographic characteristics of ARV and PrEP clients according to clients transferred by the CBO and walk in clients in Ho Chi Minh City and Dong Nai Province in 2021 (n=690)
Table 2 presents the findings on the understanding of ARV and PrEP clients about services of Community Based Organizations (CBOs). Both ARV and PrEP client groups reported that the service clients received was primarily support for transfer to treatment (100%). For ARV treatment, the majority of clients who believed that CBOs supported transfers to confirmed testing facility (84.6%) and psychological counselling (77.5%). In both ARV and PrEP client groups, the CBO supported free HIV screening testing, accounting for a high proportion (more than 70%). However, only about 50% of ARV clients received counselling on prescription adherence, which was even lower in the group of PrEP clients (20.1%). ARV clients received a wider range of services than PrEP clients. Nevertheless, PrEP clients were given more emphasis by the CBO on PrEP treatment counselling (79.8%) as compared to HIV infection counselling (62.6%).
| Variable* |
ARV1 (n=335); (n, %) |
PREP1 (n=355); (n, %) |
| Know about CBOs (Yes) |
174 (51.9) |
204 (57.5) |
| Get the support of CBOs (n=378) (Yes) |
169 (97.1) |
203 (99.5) |
| Services that clients received (multiple choice answers) |
| Support for transfer of treatment |
169 (100.0) |
185 (100.0) |
| Transfer to confirmed testing facility |
143 (84.6) |
// |
| Psychological stability counseling |
131 (77.5) |
// |
| Free HIV1 screening test |
123 (72.8) |
156 (76.8) |
| Treatment adherence counseling ̣ |
83 (49.1) |
57 (20.1) |
| Distribution of condoms and lubricants |
45 (26.6) |
120 (59.1) |
| Provide self-testing |
21 (12.4) |
109 (53.7) |
| Support for transfer of treatment for comorbidities |
11 (6.5) |
4 (2.0) |
| Support to purchase health insurance |
11 (6.5) |
// |
| Support by medication delivery service |
4 (2.4) |
// |
| Guaranteed treatment |
3 (1.8) |
// |
| Paid screening tests |
1 (0.6) |
// |
| Support for prescriptions |
1 (0.6) |
// |
| PrEP treatment counseling |
// |
162 (79.8) |
| HIV1 infection counseling |
// |
127 (62.6) |
*Collected via client response; //: Not applicable/No observation value
1Notes: ARV: Antiretroviral; PREP: Pre-Exposure Prophylaxis; HIV: Human Immunodeficiency Virus
Table 2. Understanding of ARV and PrEP clients about services of Community Based Organizations (CBOs) in Ho Chi Minh city and Dong Nai Province in 2021 (n=690).
Table 3 presents the satisfaction score of ARV and PrEP clients according to CSQ-8 scale for the CBO's services. The majority of clients were satisfied with the CBO's services. Also, PrEP clients had higher satisfaction scores than ARV clients. ARV clients reported that they will return to CBOs when they need assistance again, with the highest satisfaction score (3.7 ± 0.6). Meanwhile, the lowest satisfaction score was in the area of clients receiving the type of service they need, meeting their individual needs.
| Characteristics |
ARVa (N=174) |
PrEPa (N= 204) |
| Mean ± SD* |
Max-min** |
Mean ± SD* |
Max-min** |
| Overall assessment of service quality |
3.4 ± 0.6 |
02-04 |
3.3 ± 0.6 |
02-Apr |
| Service to be provided |
3.1 ± 0.7 |
01-04 |
3.5 ± 0.5 |
02-Apr |
| Meet individual needs |
3.1 ± 0.6 |
01-04 |
3.4 ± 0.6 |
02-Apr |
| Recommendation to others who need support |
3.6 ± 0.6 |
01-04 |
3.7 ± 0.4 |
03-Apr |
| Level of satisfaction with services |
3.3 ± 0.9 |
01-04 |
3.2 ± 0.7 |
01-Apr |
| The service received helps to solve the problem |
3.6 ± 0.5 |
03-04 |
3.8 ± 0.3 |
03-Apr |
| Overall rating of satisfaction |
3.6 ± 0.5 |
03-04 |
3.4 ± 0.6 |
01-Apr |
| Find CBOs when you need support again |
3.7 ± 0.6 |
01-04 |
3.8 ± 0.4 |
03-Apr |
| Average score of service provision satisfaction of CBOs |
3.4 ± 0.6 |
01-04 |
3.5 ± 0.6 |
01-Apr |
Note: 1. Very dissatisfied; 2. Dissatisfied; 3. Satisfied; 4. Very satisfied
*SD: Standard Deviation; **Max-Min: Maximum–Minimum
aNotes: ARV: Antiretroviral; PREP: Pre-Exposure Prophylaxis
Table 3. Satisfaction score of ARV and PrEP clients according to CSQ-8 scale for the CBO's services in Ho Chi Minh city and Dong Nai Province in 2021 (n=378).
Table 4 presents the clients perceived level of CBO's support for ARV and PrEP service. It was found that the CBO's support level for clients is quite high, averaging over 80%. In both ARV and PrEP treatment groups, the majority of clients believed that CBOs help clients with quick access to necessary services. Lastly, CBOs helped to provide motivation needed for clients to access and use health services, helping to reduce their anxiety and confusion.
| Support from CBO |
ARVa (N=174) |
PrEPa (N= 204) |
| Mean ± SD* |
Max-Min** |
Mean ± SD* |
Max-Min** |
| Motivation for accessing and using health services |
90.8 ± 18.2 |
0-100 |
88.2 ± 13.1 |
16-100 |
| Quick access to necessary services |
90.8 ± 19.4 |
0-100 |
92.4 ± 10.2 |
50-100 |
| Reducing anxiety and confusion |
89.8 ± 20.4 |
0-100 |
90.4 ± 13.6 |
20-100 |
| Better helping with treatment adherence |
89.5 ± 21.1 |
0-100 |
84.8 ± 19.9 |
0-100 |
| Peace of mind because you have a companion |
88.6 ± 23.3 |
0-100 |
89.1 ± 15.3 |
0-100 |
* SD: Standard Deviation; **Max-Min: Maximum–Minimum
aNotes: ARV: Antiretroviral; PREP: Pre-Exposure Prophylaxis.
Table 4. CBO's level of support for ARV and PrEP clients in Ho Chi Minh City and Dong Nai Province in 2021 (n=378).
Table 5 shows the association between clients transferred by CBOs, walk in, and T-lymphocyte CD4+count/stage of disease. The findingssuggest that the odds for CD4 count being higher than 200 among those clients brought in by the CBOs were 1.98 times higher than those clients who directly walked in (p=0.031). Similar, the odds for being brought into the clinic during stage I of disease were 3.18 times more for those clients who directly walked in p=0.001.
| Characteristics |
CD4# > 200
(n=197)
n (%) |
CD4 ≤ 200
(n=54)
n (%) |
p value |
OR1 (CI 95%) |
| CBO (126) |
106 (53.8) |
20 (37.0) |
0.031 |
1.98 (1.07-3.68) |
| Walk in (125) |
91 (46.2) |
34 (63.0) |
|
1 |
| Characteristics |
Stage 1^ (n=290) n (%) |
Other stages (n=45) n (%)
n (%) |
p-value |
OR (CI 95%)1 |
| CBO (169) |
154 (53.1) |
12 (26.7) |
0.001 |
3.18 (1.55-6.27) |
| Walk in (166) |
136 (46.9) |
33 (73.3) |
|
1 |
1Logistic regression; OR: Odd Ratio; CI 95%; Confidence Interval 95%; #CD4 test results for the first time ^Clinical stage for the first time
Table 5. Bivariate analysis between clients who were transferred by CBOs and walk in for T-lymphocyte CD4+count and stage of disease.
Discussion
The study aimed to assess the role of community based organizations in supporting ARV and PrEP before and during COVID-19 in Ho Chi Minh City and Dong Nai Provinces in Vietnam. The findings suggest that the strength of CBO engagement has a potential to increase the availability and utilization of HIV/AIDS related services, particularly in epidemic situations. The CBOs have an essential role in terms of early detection and transferring HIV clients to clinics on time. These findings support the international findings that CBOs add value to the national response to HIV/AIDS. This seems to be crucial in low and middle income countries, where the poorer population, less capacity to cope with HIV/AIDS. In the absence of other service providers, CBO engagement is particularly important in improving and supporting clients' reach to service availability and utilization at the community level. Most of the published literature on monitoring and evaluation of the CBOs is from high income countries. There have been limited attempts to present the findings from the evaluation of CBOs working in the low and middle income countries. Due to the resource constraints, such CBOs may find it challenging to document the effectiveness of their program [13-15].
The CBOs play a crucial role in context of care and management of HIV/AIDS. The self-initiative, knowledge, and acceptance of CBOs by the community and their relative cost effectiveness have been identified as factors that make them suitable as advocates and participants in HIV/ AIDS prevention program. Previous research has shown that the CBOs were able to offer support and help to find hard to reach populations and MSM. The CBOs are uniquely positioned to offer a bouquet of services to assist people living with or at risk of HIV/ AIDS. This includes culturally adapted programs to help people along the HIV care continuum. CBOs have contributed significantly to the improved health services access and the reduction of HIV transmission by addressing stigma and effectively mobilizing and engaging the community. The necessity to engage the CBOs in HIV/ AIDS prevention initiatives has been cited in the literature from other countries with limited resources and infrastructure [16-24].
Previous research has documented a very high rate of linkage to care (greater than 90%) for those diagnosed with HIV in the community based settings. A systematic review and meta-analysis of the evidence for community based HIV testing published articles, as recently as 2022, indicated that uptake was higher among men reached through community based HIV Testing Services (HTS) than facility based HTS. Over 70% of men reported linkage to HIV care [25]. In our study all the eligible persons were linked to the treatment service. The rate of linkage was; however, relatively lower for transfers to confirmed testing facility and psychological counselling.
It appears that those who are financially disadvantaged are more likely to reach the HIV/ AIDS care through CBOs. In the current study, the ARV clients transferred by the CBO had a lower rate of financial autonomy than the group of walk in clients. Similarly, previous research from Canada reported that the users of the Community based AIDS Service Organizations (CBAOs) were significantly poorer and more reliant on government finance/program support.
The majority of clients were satisfied with the CBO's services. The scores were relatively higher among the PrEP clients with higher satisfaction scores than ARV clients. Since the evaluation period corresponded to the COVID-19 pandemic the relevance of these findings gets even more significant. There was a substantial disruption in the HIV/AIDS related health care services during the pandemic. There was a reduction in access to prevention, testing, and treatment services as well as reduced coverage of quality essential services in Vietnam during the pandemic. In some settings in Vietnam, the patients were even diverted to the non HIV specialized facilities. The CBOs were able to deliver these services despite of facing the challenges of increased barriers to provide services during the pandemic. The CBOs were able to overcome delayed help seeking from potential clients due to various factors presenting as barriers such as quarantine, other COVID-19 prevention measures, fear of getting infected with COVID-19 from healthcare visits, and lack of information for changes in service delivery [26-28].
Despite the documented role of the CBOs, these organizations continue to face the challenge of shrinking funding opportunities. The decline in funding support for CBOs has been documented in some countries. In Vietnam, CBOs continue to remain an important stakeholder in the HIV/ AIDS prevention program. Going ahead it is important that more efficient fund utilization models and strategies are adopted by the CBOs, as recommended in the previous publications.
The study does have a few limitations in its generalizability; particularly that data was limited to two provinces. We are also not able to comment of the status of the services prior to the pandemic as that data was not available as part of the study design. Also, we could not capture the details from the patients who were not in contact of the CBOs as part of the service delivery process. However, despite of these limitations this study offers valuable insights into the role of the CBOs in the HIV/AIDS care program. There is limited literature that has documented these outcomes. It has been reported in the previous literature that the measurable effectiveness of CBOs is yet to be realized. In the setting of reduction in funding for CBOs despite their cost-effective impact highlights the importance of documenting the role of CBOs and its results in a setting of shrinking funding among vulnerable and marginalized populations. If CBOs are perceived as having limited effectiveness or an effectiveness that is yet in determined, it could be detrimental to their ability to attract funding in future. This research offers valuable information on the how CBOs play a role to offer resiliency in the setting of a public health emergency, such as the COVID-19 pandemic. There is no previously published literature from South Asia and Vietnam on this theme, which makes these findings important.
Conclusion
This study documented the role of CBOs in the HIV/AIDS program in the context of the COVID-19 pandemic in Ho Chi Minh City and Dong Nai provinces in Vietnam. The findings of the study highlight the key role played by the CBOs to facilitate clients in their seeking of care during the pandemic. There is a need to incorporate CBOs as a key stakeholder in the HIV/AIDS program in Vietnam going forward. The federal and provincial governments should leverage CBOs as a valuable resource to ensure that the HIV/AIDS program has a wider reach among the population in the country, and particularly among vulnerable and marginalized populations.
Declarations
Ethics approval and consent to participate
The study was approved by the Ethics Council of the University of Medicine and Pharmacy, Ho Chi Minh City, Decision No. 472/HDDD-DHYD, dated September 21, 2021.
Competing interests
The authors declare that they have no competing interests
Acknowledgments
We would like to thank all clients for the time and effort they devoted to this study. We greatly appreciate 4 community based organizations in sample finding and 6 ARV clinics in Ho Chi Minh City and Dong Nai Province including OPC Long Thanh, Dong Nai Clinic; District 11, 3, 4, Tan Binh District; Galant, AloCare, Glink Ho Chi Minh City, and Glink Dong Nai Province. We also gratefully acknowledge the support of CDC Ho Chi Minh City and CDC Dong Nai. We would like to thank colleagues in the South Vietnam HIV addiction technology transfer centre and Ho Chi Minh City HIV/AIDS centre for contributions this research.
References
- Summary report on HIV/AIDS prevention and control in 2020. Vietnam Administration of HIV/AIDS Control. 2020.
- Underhill K, Morrow KM, Colleran C, Calabrese SK, Operario D, et al. Explaining the Efficacy of Pre-Exposure Prophylaxis (PrEP) for HIV Prevention: A Qualitative Study of Message Framing and Messaging Preferences among US Men Who Have Sex with Men. AIDS Behav. 2016;20(7):1514–1526.
[Crossref] [Google Scholar] [PubMed]
- Dave S, Peter T, Fogarty C, Karatzas N, Belinsky N, et al. which community based HIV initiatives are effective in achieving UNAIDS 90-90-90 targets? A systematic review and meta-analysis of evidence (2007-2018). PLOS ONE. 2019;14(7):0219826.
[Crossref] [Google Scholar] [Pubmed]
- Bailey ME. Community based organizations and CDC as partners in HIV education and prevention. Public Health Rep. 1991;106(6):702–708.
[Google Scholar] [PubMed]
- DiNenno EA. Recommendations for HIV screening of gay, bisexual, and other men who have sex with men united states, 2017. MMWR Morb Mortal Wkly Rep. 2017
- Akbari A, Mayhew A, Al‐Alawi MA, Grimshaw J, Winkens R, et al. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database Syst Rev. 2005.
- Pinto RM, Park S. COVID-19 pandemic disrupts HIV continuum of care and prevention: Implications for research and practice concerning community based organizations and frontline providers. AIDS Behav. 2020;24(9):2486–2489.
[Crossref] [Google Scholar] [PubMed]
- Mayberry RM, Daniels P, Yancey EM, Akintobi TH, Berry J, et al. Enhancing community-based organizations capacity for HIV/AIDS education and prevention. Eval Program Plann. 2009; 32(3):213–220.
[Crossref] [Google Scholar] [PubMed]
- Nguyen Thu H, Nguyen Quynh A, Khuat Hai O, Le Thi Thanh H, Nguyen Thanh H. Impact of the COVID-19 pandemic on provision of HIV/AIDS services for key populations. Int J Health Plan Manag. 2022;37(5):2852–2868.
[Crossref] [Google Scholar] [PubMed]
- Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10(5):348–354.
[Crossref] [Google Scholar] [PubMed]
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: Development of a general scale. Eval Program Plann. 1979;2(3):197–207.
[Crossref][Google Scholar][Pubmed]
- Meulbroek M, Ditzel E, Saz J, Taboada H, Perez F, et al. BCN Checkpoint, a community based centre for men who have sex with men in Barcelona, Catalonia, Spain, shows high efficiency in HIV detection and linkage to care. HIV Med. 2013;14(3):25–28.
[Crossref] [Google Scholar] [PubMed]
- Richter DL, Prince MS, Potts LH, Reininger BM, Thompson MV, et al. Assessing the HIV prevention capacity building needs of community-based organizations. J Public Health Manag Pract. 2000;6(4):86–97.
[Crossref] [Google Scholar] [PubMed]
- Williams P, Narciso L, Browne G, Roberts J, Weir R, et al. Characteristics of people living with HIV who use community-based services in Ontario, Canada: implications for service providers. J Assoc Nurses AIDS Care. 2005; 16(4):50–63.
[Crossref] [Google Scholar] [PubMed]
- Lorente N, Preau M, Vernay-Vaisse C, Mora M, Blanche J, et al. Expanding access to non-medicalized community-based rapid testing to men who have sex with men: An urgent hiv prevention intervention. PLOS ONE. 2013;8(4):61225.
[Crossref] [Google Scholar] [PubMed]
- Bogart LM, Wagner GJ, Mutchler MG, Risley B, McDavitt BW, et al. Community HIV treatment advocacy programs may support treatment adherence. AIDS Educ Prev. 2012;24(1):1–14.
[Crossref] [Google Scholar] [PubMed]
- Gelaude DJ, Sovine ML, Swayzer R, Herbst JH. HIV prevention programs delivered by community based organizations to young transgender persons of colour: Lessons learned to improve future program implementation. Int J Transgend. 2013;14(3):127–139.
[Crossref] [Google Scholar]
- Krivelyova A, Kakietek J, Connolly H, Bonnel R, Manteuffel B, et al. Funding and expenditure of a sample of community based organizations in Kenya, Nigeria, and Zimbabwe. AIDS Care. 2013;25(1):20–29.
[Crossref] [Google Scholar] [PubMed]
- Rodriguez-Garcia R, Wilson D, York N, Low C, Bonnel R. Evaluation of the community response to HIV and AIDS: Learning from a portfolio approach. AIDS Care. 2013; 25(1):7–19.
[Crossref] [Google Scholar] [PubMed]
- Campbell C, Scott K, Nhamo M, Nyamukapa C, Madanhire C, et al. Social capital and HIV Competent Communities: The role of community groups in managing HIV/AIDS in rural Zimbabwe. AIDS Care. 2013; 25(1):114–122.
[Crossref] [Google Scholar] [PubMed]
- Williamson RT, Rodd J. Civil society advocacy in Nigeria: Promoting democratic norms or donor demands? BMC Int Health Hum Rights. 2016;16(1):19.
[Crossref] [Google Scholar] [PubMed]
- Akeju D, Nance N, Salas-Ortiz A, Fakunmoju A, Ezirim I, et al. Management practices in community based HIV prevention organizations in Nigeria. BMC Health Services Res. 2021;21(1):489.
[Crossref] [Google Scholar] [PubMed]
- Groves AK, Stankard P, Bowler SL, Jamil MS, Gebrekristos LT ,et al. A systematic review and meta-analysis of the evidence for community based HIV testing on men’s engagement in the HIV care cascade. Int J STD AIDS. 2022;33(13):1090–1105.
[Crossref] [Google Scholar] [PubMed]
- Jewell BL, Mudimu E, Stover J, Brink D ten, Phillips AN, et al. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: results from multiple mathematical models. The Lancet HIV. 2020;7(9):629–640.
[Crossref] [Google Scholar] [PubMed]
- Yang X, Zeng C, Tam CC, Qiao S, Li X, et al. HIV service interruptions during the COVID-19 Pandemic in China: The Role of COVID-19 challenges and institutional response from healthcare professional’s perspective. AIDS Behav. 2022;26(4):1270–1278.
[Crossref] [Google Scholar] [PubMed]
- Schwartlander B, Stover J, Hallett T, Atun R, Avila C, et al. Towards an improved investment approach for an effective response to HIV/AIDS. The Lancet. 2011; 377(9782):2031–2041.
[Crossref] [Google Scholar] [PubMed]
- Kegeles SM, Rebchook G, Pollack L, Huebner D, Tebbetts S, et al. An intervention to help community based organizations implement an evidence based hiv prevention intervention: The empowerment project technology exchange system. Am J Community Psychol. 2012;49(1–2):182–98.
[Crossref] [Google Scholar] [PubMed]
- Onwujekwe O, Ezumah N, Mbachu C, Obi F, Ichoku H, et al. Exploring effectiveness of different health financing mechanisms in Nigeria; what needs to change and how can it happen? BMC Health Services Res. 2019; 19(1):661.
[Crossref] [Google Scholar] [PubMed]