Abstract
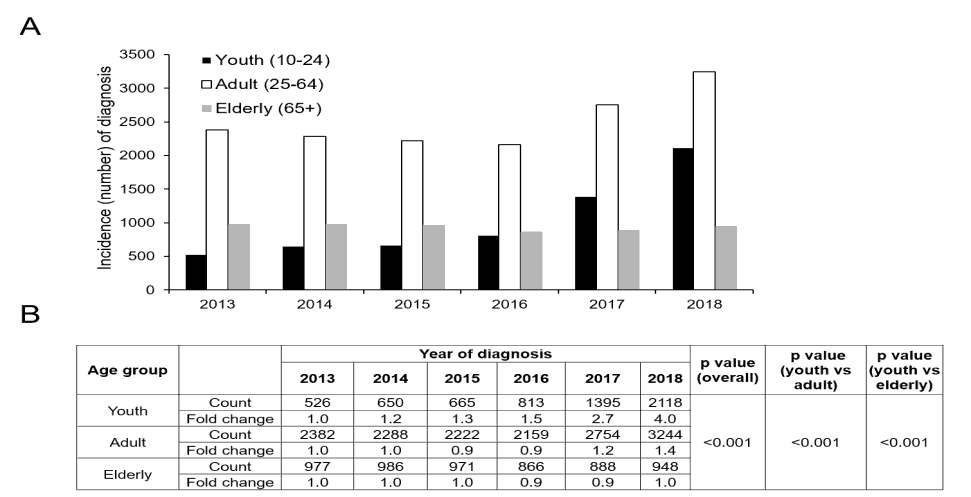
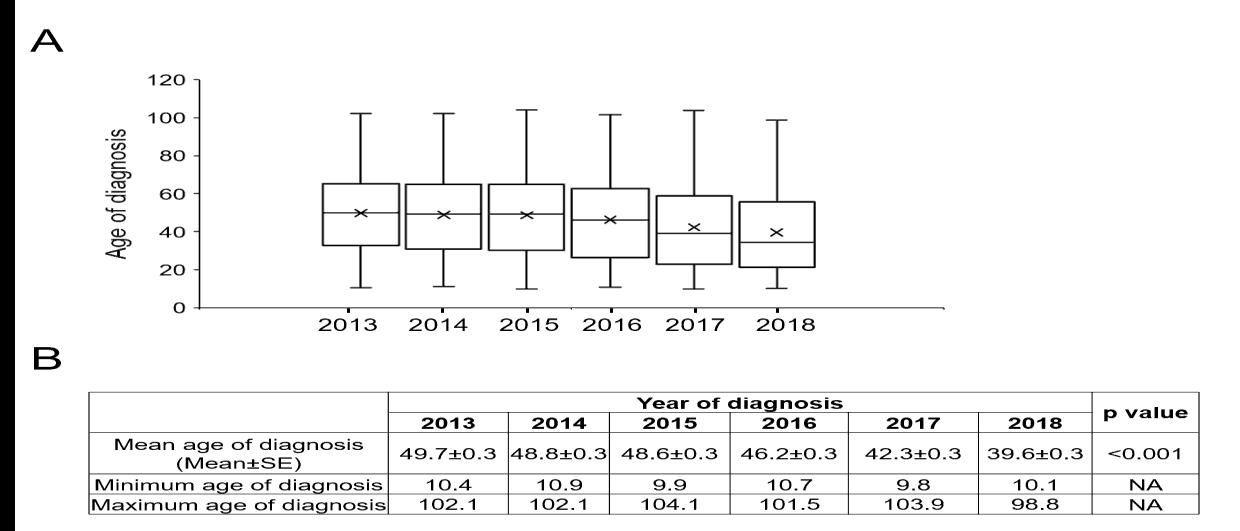
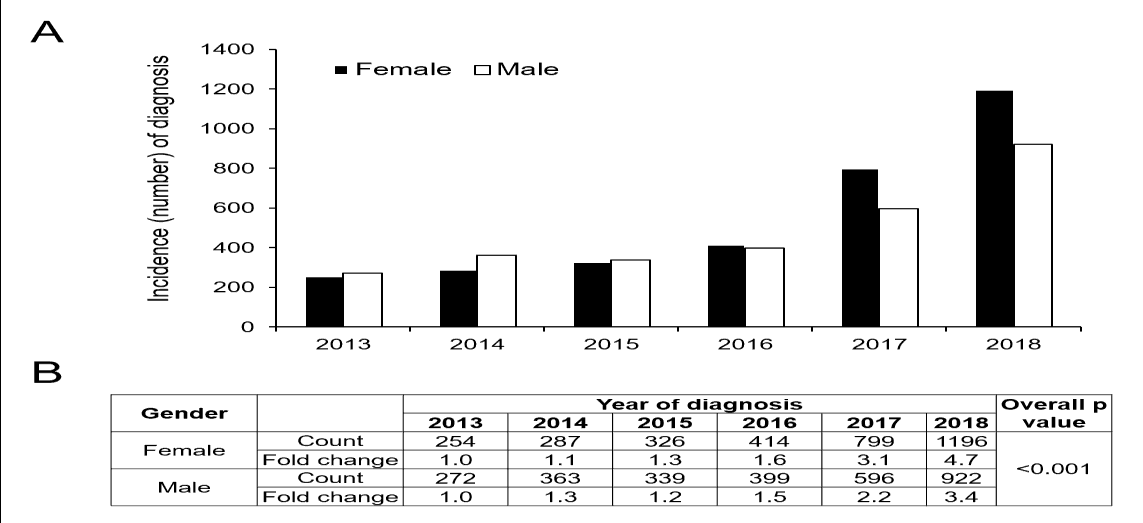
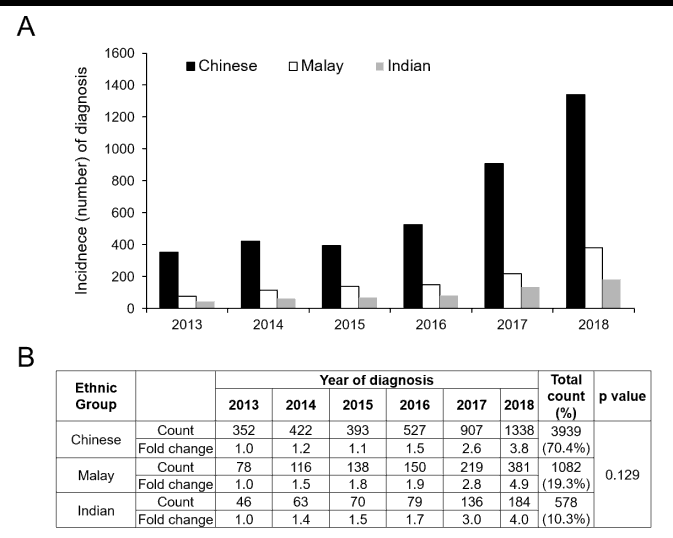
Aim: To examine the trend of youth depression diagnosed in a healthcare group in Singapore over a 6-year period. Methods: This is a retrospective analysis of the medical records of patients who had been diagnosed with depression from Jan 2013 to Dec 2018 in a healthcare group in Singapore. The yearly trend of depression diagnosis among the youths (10-24 years of age) was compared with adults (25-64 years of age) and the elderly (≥ 65 years of age). The mean age at diagnosis, distribution of gender, ethnicity and clinical care settings among the subgroup of youth patients were compared across the years using analysis of variance or Pearson’s chi-square test. Results: A total of 4701 youths, 15243 adults and 6908 elderly patients were included in the analysis. Between 2013 and 2018, the rise in depression diagnosis in the youth was greater than in the adult and elderly populations, and the mean age at diagnosis decreased from 49.7 ± 0.3 (mean ± SE) years in 2013 to 39.6 ± 0.3 years in 2018. Among the youths, more females had been diagnosed with depression than males and females displayed a larger increase in diagnosis of depression. There was also a larger increase in the diagnosis of depression in primary care compared to emergency departments, outpatient specialist clinics and in-hospital wards. Conclusion: Youth depression is a major health problem in Singapore. There is a need for the expansion of resources in a variety of avenues for depressed youths to seek help.
Keywords
Youth Depression, Incidence of Diagnosis, Age of Diagnosis, Gender Related Depression, Trend Analysis
Introduction
Adolescence is a period of sensitive growth, involving profound changes in all domains of development—biological, cognitive, psychosocial, emotional and behavioural [1]. The challenges of youths are manifold: separation from family and the development of independence, handling peers and the pressures that come with that and, the development of a self-identity to better cope with the future, all while growing up in volatile, uncertain, complex and ambiguous environments [2]. Today’s youths face significant pressures, ranging from disturbances in family life, academic endeavours, school/internet bullying and body image issues [3]. Multiple physical, emotional and social changes, including exposure to hormonal changes of puberty, family abuse, or violence, can also make a youth vulnerable to mental health problems such as depression, which frequently results in serious consequences such as dropping out of school, [4] substance abuse, [5,6] suicidal ideation [7,8] eating disorders as well as illnesses such as obesity [9,10].
The prevalence of depression in younger people is increasing globally [11-13]. Little information on the economic burden of depression in childhood is currently available, though the overall societal cost per child with depression is increasing annually and is linked to a large extent with loss of productivity [14]. Thus, promoting healthy psychosocial environments for growth and protecting youths from adverse life experiences and risks that may impact their growth are critical for their well-beings during adolescence and physical and mental health later during adulthood. However, the early detection, diagnosis and treatment of depressive disorders in youth remains challenging for various reasons, including lack of awareness, stigma towards psychiatric illness, difficulty in obtaining consent from parents/guardians and difficulty in differentiating normal mood fluctuations from persistent mood and behavioural changes [15]. The rise in cases of tragic youth suicide and school violence urges parents, schools and society as a whole to pay more attention to the mental health burden of our youth.
Singapore is one of the countries with the highest burden of mental health issues in Asia in recent years. The second Singapore Mental Health Study, conducted in 2016, revealed a significant association between younger age and mental disorders [16]. The prevalence of youths suffering from mental disorders increases every year [17]. Rates of clinically elevated symptoms of anxiety and depression were reported by a 2015 survey study to be 9.3% and 16.9% respectively among 8-12 year-old Singaporean children [18]. Recognizing the early warning signs of depression and actively seeking psychiatric counselling or other treatment options are critical to help youths suffering from depressive symptoms. The aim of our study was to examine the yearly trend, age of diagnosis and the impact of gender, ethnicity and clinical care setting on the incidence of depression among patients less than 25 years old between January 2013 to December 2018.
Methods
Participants
We extracted patients’ medical information from electronic health records via the Chronic Disease Management System (CDMS). The CDMS is a purposefully-built database for patients with chronic conditions and facilitates the provision of comprehensive and evidence-based population management. It contains the longitudinal healthcare information of patients who have visited any of the 17 hospitals/polyclinics under the National Healthcare Group (NHG). The details of CDMS and the method of data extraction can be found in our previous report [19]. For this study, we extracted the information of patients whose diagnosis of depression have been newly registered into CDMS between 01 January 2013 and Dec 31, 2018. Diagnoses were defined by the International Classification of Diseases (ICD)-10 or Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV or DSM 5 criteria. Ethical approval to conduct the study was obtained from the NHG Domain Specific Review Board (2019/00944). A waiver of patient’s informed consent was granted as data was retrospectively collected without disclosure of patients’ identities.
Statistical analysis
Patients aged 10 to 24 years were categorised as the “youth” group [15]; patients aged 25 to 64 years were categorized as the “adult” group and patients aged 65 years or above were categorized as the “elderly” group [20,21]. The mean age of diagnosis of all patients was compared across years via Analysis Of Variance (ANOVA). The total counts of depression diagnoses per year were compared between the three age groups using Pearson’s Chi-square test. Annual incidence of depression (yes/no) in the “youth” subgroup was further stratified by gender, ethnicity and clinical care setting and compared with Pearson’s Chi-square test. Fold changes of annual incidence was calculated by dividing the yearly counts by the number of diagnoses at baseline (year 2013).
Results
A total of 26852 depressive patients including 4701 (17.5%) youths, 15243 (56.8%) adults and 6908 (25.7%) elderly patients were included in the analysis. The yearly incidence of depression of the three age groups were plotted in (Figure 1A). Starting from the baseline number in 2013, the fold change of depression incidence gradually increased to 4.0 for the youths, 1.4 for the adults and remained at 1.0 for the elderly patients in 2018 (Figure 1B). The relative growth of the incidence of depression from baseline year 2013 was greater among the youths compared to the adults and the elderly patients (p<0.001). The mean age of diagnosis decreased from 49.7 ± 0.3 (mean ± SE) years in 2013 to 39.6 ± 0.3 years in 2018 (Figure 2A and 2B, overall p<0.001).
We examined the yearly incidence of depression by gender in the youth group (Figure 3A). Starting from the baseline number in 2013, the fold change of incidence of depression gradually increased to 4.7 for females and 3.4 for males respectively in 2018 (Figure 3B). Compared to male patients, there was a significantly larger increase in depression incidence in the female patients (p<0.001).
The yearly trend of depression incidence by ethnicity in the youth group was plotted in (Figure 4A). Starting from the baseline number in 2013, the fold change of depression incidence gradually increased to 3.8 for the Chinese, 4.9 for the Malays and 54.0 for the Indians in 2018 (Figure 4B), with no significant difference in the rate of growth between the ethnic groups (p=0.129).
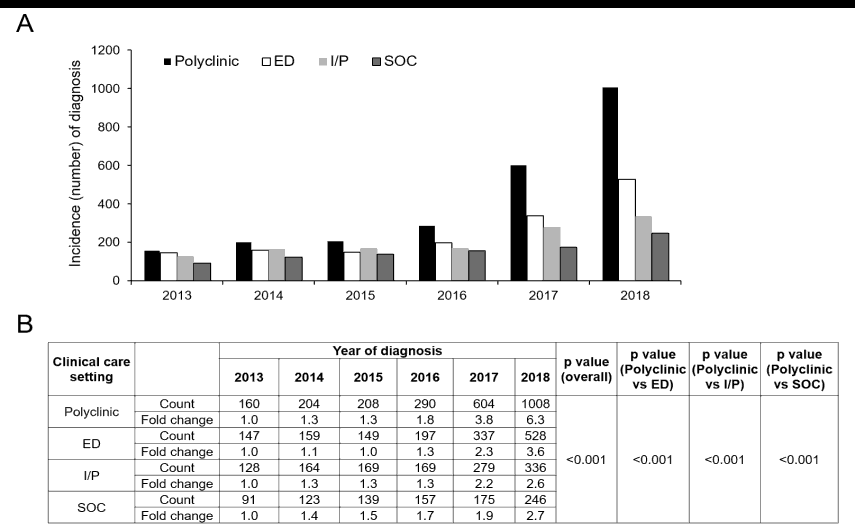
Finally, we examined the yearly trend of depression incidence by clinical care setting in the youth patient group (Figure 5A). Starting from the baseline number in 2013, the fold change of depression diagnosis gradually increased to 6.3 in polyclinics, 3.6 in emergency departments, 2.6 in inpatient wards and 2.7 in specialist outpatient clinics in 2018 (Figure 5B). There was statistically significant difference in the incidence of depression diagnosis among polyclinics compared to other clinical care settings (p<0.001).
Discussion
In this study, by examining a population of patients with newly diagnosed depression over a 6-year period within a Singapore healthcare group consisting of primary care, general hospitals and a specialist tertiary psychiatry centre, we found that there was a more rapid increase in the diagnosis of depression among youths compared to adults and the elderly. The mean age at first diagnosis also reduced over the 6 years. Moreover, more girls had been diagnosed with depression than boys and girls displayed a higher rate of increase. Finally, more patients had been diagnosed in polyclinics while fewer in emergency departments, outpatient specialist clinics and in-hospital wards.
Similar to the increasing incidence of depression among youths in other countries, [22] more young patients in Singapore are being diagnosed with depression. Many causes have been proposed to account for youth mental illness. One reason for the increase in diagnosis of depression is possibly the advent of community mental health education in recent years, which has improved public awareness of mental illness and encouraged help-seeking behaviour. In Singapore, many social interventions are introduced to combat youth depression. In 2018, the Ministry of Education in Singapore announced changes to its grading systems for school examinations, intended to ease academic pressure. Starting from 2021, mental health lessons have been incorporated into the student development curriculum [23]. Students have learned about common mental health problems, how to recognise signs of distress and where to find help. These lessons have helped to strengthen students’ resilience and well-being, fostered help-seeking behaviour and encouraged students to develop empathy and caring for those with mental illness.
Youth depression may represent the start of a chronic illness and are often associated with impairments in psychosocial functioning in adulthood, [24] suggesting that a possible reason for the increasing incidence of adult depression in recent years could be missed diagnoses in youth. In contrast, the yearly number of depression diagnosis remains steady in the elderly from 2013 to 2018 despite Singapore facing an increasingly aging population [25]. This is in keeping with previous observations that the prevalence of depression in the elderly population in Singapore has decreased as compared to a decade ago [26]. This success can possibly be attributed to the various national efforts initiated in the early of 2000’s, targeted at achieving “Successful Ageing in Singapore”. Nevertheless, compared to the adults and the elderly, the rapid increase in diagnosis of depression in youths translates into a growing number of young people with depression remaining untreated. Moreover, the yearly number of new diagnosis of youth depression in our study sample is much lower than the reported prevalence of depression among the youth in Singapore. This treatment gap highlights the need to address depression at an earlier age by continuously promoting help-seeking and uptake of treatment in the younger population.
It is widely accepted that teenagers can experience clinical depression while the age of onset of depression could be even younger [27]. Earlier onset of depression is associated with multiple markers of greater illness burden. Compared to adult-onset depression, adolescent-onset depression has been found to be associated with greater psychosocial impairment, physical health problems, psychiatric comorbidity, and suicidality [28,29]. With the age of onset becoming younger, early interventions are critical and studies are needed to evaluate various forms of psychotherapy and psychopharmacology for this age group. Patients with mild illness symptoms may need non-medical interventions such as cognitive behaviour therapies.
Mental illness, including depression, is more common in girls. Studies suggest that female youths may be more susceptible to particular types of stressors, particularly the quality of the parent-child relationship [30-32]. Consistent with these reports, we observed that more female patients had been diagnosed with depression per year compared to male patients in the youth subpopulation. Moreover, female patients recorded a larger increasing rate of depression diagnosis over the 6 years compared to male patients. This discrepancy suggests that the impact of psychosocial stressors, such as family support, friendships and poor health condition, is greater in females than males over this period of growth. Another explanation is possibly the difference in depressive symptomatology between the genders. While depressed boys are more likely to present with irritability, fatigue, trouble in sleeping and loss of pleasure depressed girls tend to present with sadness, guilt, difficulty in concentration, dissatisfaction with body image and low energy [33] which are possibly more easily recognised by their family members or members of their social circles. This discrepancy suggests that the treatment interventions for depression may need to have different targets for either gender: for example, excessive guilt and self-hatred in girls and suicidal ideation and substance abuse in boys.
Singapore is a multiracial and multicultural country, with ethnic Chinese (76.2% of the citizen population), Malays (15.0%), and ethnic Indians (7.4%) making up the population, as reported in 2014 [34]. In our study, we observed there was an overall higher proportion of Malay (19.3%) and Indian youths (10.3%) while less Chinese youths (70.4%) diagnosed with depression compared to the general ethnicity distribution in Singapore population in 2014. As there are no prior reports of the prevalence of depression among the youth population stratified by ethnicity, the reason behind this observation remains unclear.
There was a larger increase in number of new depression diagnosis among youth patients in the polyclinic setting compared to the outpatient specialist clinics and inpatient wards. This is consistent with a recent report noting that as more cases of youth depression are picked up in community settings or by community organisations, fewer youths have been seeking help at the specialist clinics in tertiary institutions [35]. This suggests that many cases are being managed in the community or by the REACH (Response, Early intervention and Assessment in Community mental Health) team, which is a mental healthcare service set up to work closely with schools, Voluntary Welfare Organizations (VWOs), and General Practitioners (GPs) in Singapore to help students with emotional, social and/or behavioural issues within the community [36]. The emergency department ranked second for the rate of increase of diagnosis of depression. This suggests that despite the community interventions as stated above, there is still a high prevalence of emergency presentations related to depression, such as suicide attempts, alcohol/illicit substance abuse or aggressive/violent behaviour in the youth population. It is notable that the majority of youths who die by suicide have never received any type of psychiatric treatment or mental health service [37,38]. This suggests that there is still a treatment gap with regards to identifying and managing youth depression in the community. More efforts are therefore needed to facilitate early screening, diagnosis and treatment for youths at high risk of depression.
In this study, we extracted and analysed information from a large number of hospitals/clinics that served the whole population of Singapore. Therefore, our data is representative of the general population of youths with depression in Singapore. The major limitation of our study is that some of the diagnoses of depression in electronic health records were generated in community settings via unstructured Traditional Diagnostic Assessment (TDA), which may not be accurate as compared to diagnosis generated by standardized/structured interviews. However, as the first medical contact, an early and quick identification of the warning signs of depression by unstructured TDA are particularly important for an early prevention and intervention for those patients in need.
Conclusion
In summary, based on data from the electrotonic medical records deposited in CDMS from 2013 to 2018, we observed a more rapid increase in depression diagnosis in youths, as compared to adults and the elderly. Moreover, the mean age of diagnosis became younger over the period, with a larger increase in depression diagnosis in young females compared to males. Additionally, more patients were diagnosed in polyclinics compared to emergency departments, outpatient specialist clinics and inpatient wards. These findings suggest that more can be done to identify, diagnose and treat youth depression in the community. Greater efforts are required to expand screening and assessment programmes and develop more innovative treatments to best meet the mental health needs of these young patients.
Author Contributions
XWT, DS formulated the research questions; XWT, ESL, KKL, PCT and DF designed the study; XWT, MT collected the data; XWT, PCT and DF analysed the data; TXW, DF wrote first draft of the article and all authors reviewed and agreed the submission of the manuscript in current version.
Data Availability Statement
The data that support the findings of this study is not publicly available and is only accessible via approval by the Institutional Research Review Committee and the National Healthcare Group Domain Specific Review Board.
References
- National Academies of Sciences E, and Medicine; Division; HaM, Education; DoBaSSa, Board on Children Y, and Families; Applications CotNaS-bSoADaI. The Promise of Adolescence: Realizing Opportunity for All Youth. Washington (DC): National Academies Press (US) 2019.
- Noda Y. Socioeconomically transformation and mental health impact by the COVID-19's ultimate VUCA era: Toward the New Normal, the New Japan, and the New World. Asian Journal of Psychiatry. 2020; 54: 102-262.
- Garber J. Depression in children and adolescents: Linking risk research and prevention. American Journal of Preventive Medicine. 2006; 31(6): S104-125.
- Fletcher JM. Adolescent depression: Diagnosis, treatment, and educational attainment. Health Econ. 2008; 17: 1215-1235.
- Aseltine RH, Gore S, Colten ME. The co-occurrence of depression and substance abuse in late adolescence. Development and Psychopathology. 1998; 10: 549-570.
- Levy JC, Deykin EY. Suicidality, depression, and substance abuse in adolescence. US: American Psychiatric Assn. 1989; 146(11): 1462-1467.
- Hawton K, Heeringen K. Suicide. Lancet. 2009; 373: 1372-1381.
- Windfuhr K, David W, Isabelle H, Pauline T, Rebecca L, et al., Suicide in juveniles and adolescents in the United Kingdom. The Journal of Child Psychology and Psychiatry. 2008; 49(11): 1155-1165.
- Hasler G, Pine DS, Kleinbaum DG, Gamma A, Luckenbaugh D et al. Depressive symptoms during childhood and adult obesity: The Zurich Cohort Study. Molecular Psychiatry. 2005; 10: 842-850.
- Keenan-Miller D, Hammen CL, Brennan PA. Health outcomes related to early adolescent depression. Journal of Adolescent Health. 2007; 41: 256-262.
- Lu Wenhua. Adolescent Depression: National Trends, Risk Factors, and Healthcare Disparities. American Journal of Health Behavior. 2019; 43(1): 181-194.
- Thorisdottir IE, Asgeirsdottir BB, Rannveig S, Allegrante J, Sigfusdottir I. The increase in symptoms of anxiety and depressed mood among Icelandic adolescents: time trend between 2006 and 2016. The European Journal of Public Health. 2017; 27: 856-861.
- Wiens K, Bhattarai A, Pedram P, Dores A, Williams J, et al., A growing need for youth mental health services in Canada: examining trends in youth mental health from 2011 to 2018. 2020; 29: e115.
- Chisholm D. The economic consequences of depression; Dawson A, Tyle A, editors. London: British Medical Journal Books on behalf of the WHO Regional Office for Europe. 2001; p: 121.
- Medicine SfAHa, Young adult health and well-being: A position statement of the society for adolescent health and medicine. J Adolesc Health. 2017; 60: 758-759.
- Subramaniam M, Abdin E, Vaingankar JA, Shafle S, Chua BY, et al., Tracking the mental health of a nation: Prevalence and correlates of mental disorders in the second Singapore mental health study. Epidemiol Psychiatric Science. 2019; 29: e29.
- Harish SS, Ganesh KK, Ping LY, Swapna KV, et al., A decade of influence in the Singapore youth mental health landscape: The Community Health Assessment Team (CHAT). Singapore Medical Journal. 2021; 62: 225-229.
- Magiati I. Self-reported depression and anxiety symptoms in school-aged Singaporean children. Asia Pac Psychiatry. 2015; 7(1): 91-104.
- Matthia T, Insights from health data - the national healthcare group chronic disease management system. International Journal of Integrated Care. 2019; 19: 447.
- Organization WH, Definition of an older or elderly person. 2013.
- Orimo H, Hideki I, Suzuki Takao, Atsushi A, Takayuki H, et al., Reviewing the definition of “elderly”. Geriatrics & gerontology international. 2006; 6(3): 149-158.
- Mojtabai R, Olfson M, Han B. National Trends in the Prevalence and Treatment of Depression in Adolescents and Young Adults. Pediatrics. 2016; 138(6): e 20161878.
- Co C. Schools to offer mental health lessions from 2021; more trips to Asia countries. Channel New Asia. Singapore: Singapore Mediacorp News. 2020.
- Wilson S, Hicks BM, Foster KT, Mcgue M, Iacono WG, et al., Age of onset and course of major depressive disorder: associations with psychosocial functioning outcomes in adulthood. Psychology Medical. 2015; 45(3): 505-514.
- Subramaniam M, Edimansyah A, Sambasivam R, Janhavi AV, Picco L, et al., Successful ageing in Singapore: prevalence and correlates from a national survey of older adults. Singapore Medical Journal. 2019; 60(1): 22-30.
- Subramaniam M, Abdin E, Sambasivam R, Janhavi AV, Picco L, et al., Prevalence of Depression among Older Adults-Results from the Well-being of the Singapore Elderly Study. Ann Acad Medical Singapore. 2016; 45: 123-133.
- Bernaras E, Jaureguizar J, Garaigordobil M. Child and adolescent depression: A Review of Theories, Evaluation Instruments, Prevention Programs, and Treatments. Frontiers in Psychology. 2019; 10.
- Hammen C, Patricia AB, Danielle KM, Nathaniel RH. Early onset recurrent subtype of adolescent depression: Clinical and psychosocial correlates. J Child Psychol Psychiatry. 2008; 49: 433-440.
- Zisook S, John R, Maurizio F. Effect of age at onset on the course of major depressive disorder. The American Journal of Psychiatry. 2007; 164: 1539-1546.
- Bennett DS. Gender differences in adolescent depression: do symptoms differ for boys and girls. Journal of Affect Disorders. 2005; 89: 35-44.
- Lewis AJ, Kremer P, Douglas K, Toumborou JW, Hameed MA, et al. Gender differences in adolescent depression: Differential female susceptibility to stressors affecting family functioning. Australian Journal of Psychology. 2015; 67: 131-139.
- McGuinness TM, Dyer JG, Wade EH. Gender differences in adolescent depression. Journal of Psychosocial Nursing Mental Health Services. 2012; 50(12): 17-20.
- Khesht-Masjedi MF, Somayeh S, Elahe A, Mahbuobe G, Sharif-Ghaziani Z. Comparing depressive symptoms in teenage boys and girls. Journal of Family Medicine and Primary Care. 2017; 6(4): 775-779.
- National Population and Talent Division PMsO 2014 Population in Brief. Singapore. 2014.
- Han GY. Fewer youth seeking help at IMH in recent years, more turning to community services. The straits times. Singapore Singapore New Mediacorp. 2021.
- Lim CG, Ong SH, Chin CH. Child and adolescent psychiatry services in Singapore. Child and Adolescent Psychiatry and Mental Health. 2015; 9(1): 7.
- Brent DA. Risk factors for adolescent suicide. A comparison of adolescent suicide victims with suicidal inpatients. Archives of General Psychiatry. 1988; 45(6): 581-588.
- Marttunen MJ, Aro HM, Lönnqvist JK. Adolescent suicide: Endpoint of long-term difficulties. Journal of the American Academy of Child Adolescent Psychiatry. 1992; 31(4): 649-654.